Capturing a Crisis: Weekly Behavioral Health Boarding Reports

Behavioral Health (BH) boarding occurs when a patient must wait in an emergency department (ED) or medical-surgical floor until a BH bed is available. While boarding was a major issue for Massachusetts patients and hospitals before the pandemic, the effects of COVID-19 and increasing workforce shortages have worsened the situation and intensified the behavioral health crisis.
For years, the behavioral health system in Massachusetts and nationally has struggled with serious challenges relating to patient access, inadequate reimbursement, and workforce vacancies. The long-term effects of the COVID-19 pandemic and increased need for BH services continue to exacerbate these issues. Healthcare providers are also seeing a rising acuity of patients’ behavioral health presentations, making the challenges facing the behavioral health system – including the paucity of clinical and support staff – more complex. EDs and medical-surgical units were not designed to handle the long-term needs of acute behavioral health patients, yet these settings now serve as the last available refuge for patients as they await appropriate placement.
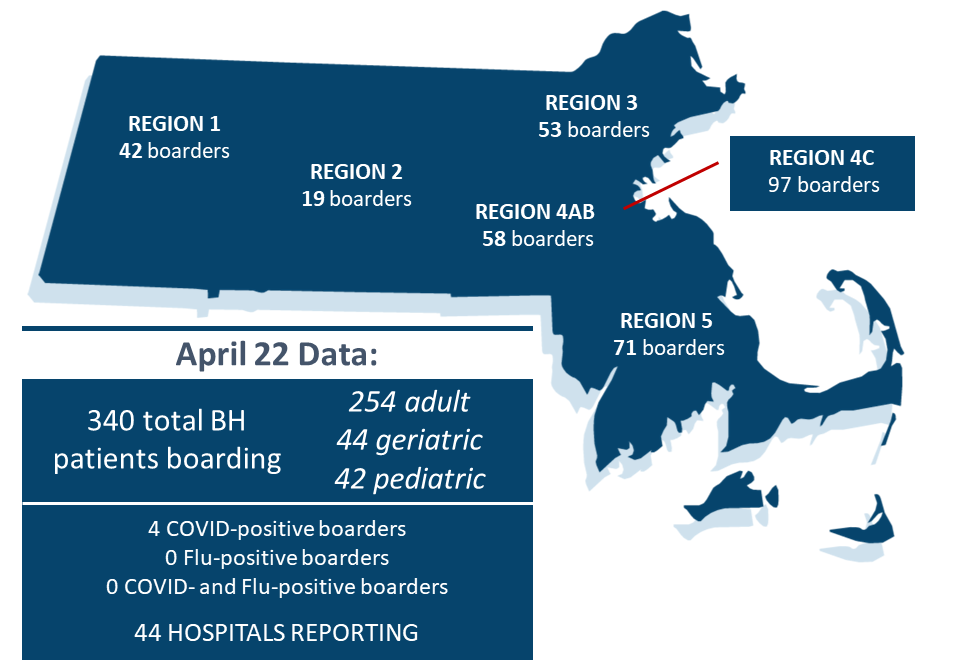
This report examines both weekly and trending data from Massachusetts acute care hospitals on the number of behavioral health patients who are waiting for a psychiatric evaluation or who have had an evaluation and are awaiting a bed. The information is further broken down by patient age, and geographic region, and effect on staffed ED bed capacity.
Addressing the behavioral health boarding challenge will require a coordinated effort to:
- increase physical capacity;
- bolster and expand the entire behavioral healthcare workforce, including entry level mental health worker positions, as well as nurses, social workers, psychiatrists, and more; and
- ensure the financial stability of behavioral health units and facilities.
Through partnership with the Executive Office of Health and Human Services and the state legislature, the inpatient psychiatric system added nearly 450 new inpatient psychiatric beds in 2021 and 2022, including both in psychiatric units at acute care hospitals and in freestanding psychiatric facilities, with additional beds to come in 2023. But fully staffing existing and newly licensed beds is a considerable barrier to opening new or expanded services. Much more needs to be done to ensure behavioral health patients have access to needed care, in particular by increasing the pipeline of staff, improving retention, and ensuring the sustainability of services.
Recent Weekly Reports
Identified solutions to address the remaining behavioral health challenges include:
Ensuring hospitals are reimbursed for the care they provide to behavioral health patients accessing care in the ED, including commercial coverage for BH crisis evaluations and services provided to patients while they board. This provides facilities with the staffing and programmatic resources needed to care for those patients.
Continued development of the behavioral health workforce pipeline across all positions, including the use of American Rescue Plan Act funds in the Behavioral Health Trust Fund.
Creation of a Behavioral Health Rate Task Force to evaluate ways to ensure the financial stability of behavioral health units and facilities, and to allow behavioral health providers to pay their workforce adequate salaries.
Prohibiting clinical denials due to an administrative or technical defect in a claim, and requiring coverage of all medically necessary mental health services.
Reducing continuum of care challenges that create bottlenecks in the behavioral health system and limit patient access to needed services. Solutions include expanding availability of continuing care services, post-acute care transitions, community wraparound services, and congregate care programs.
Addressing administrative barriers such as Determination of Need requirements for providers expanding BH services, and insurance prior authorization/notification processes for providers.
MHA will continue to work collaboratively with its members, our partners in the behavioral health space, and the state to improve behavioral healthcare in these areas.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association