INSIDE THE ISSUE
> Hospital Temp Labor: $1.52 Billion in FY22
> Time to Review the Benchmark
> Preparing for Cyber Attacks
> State Extends Capacity Plan
> FOCUS ON WORKFORCE: Tufts Medicine
> Biden’s Medicare Proposals
> DEA’s Telehealth Proposals
> Sen. Markey’s Opioid Treatment Bill
> Transition
MONDAY REPORT
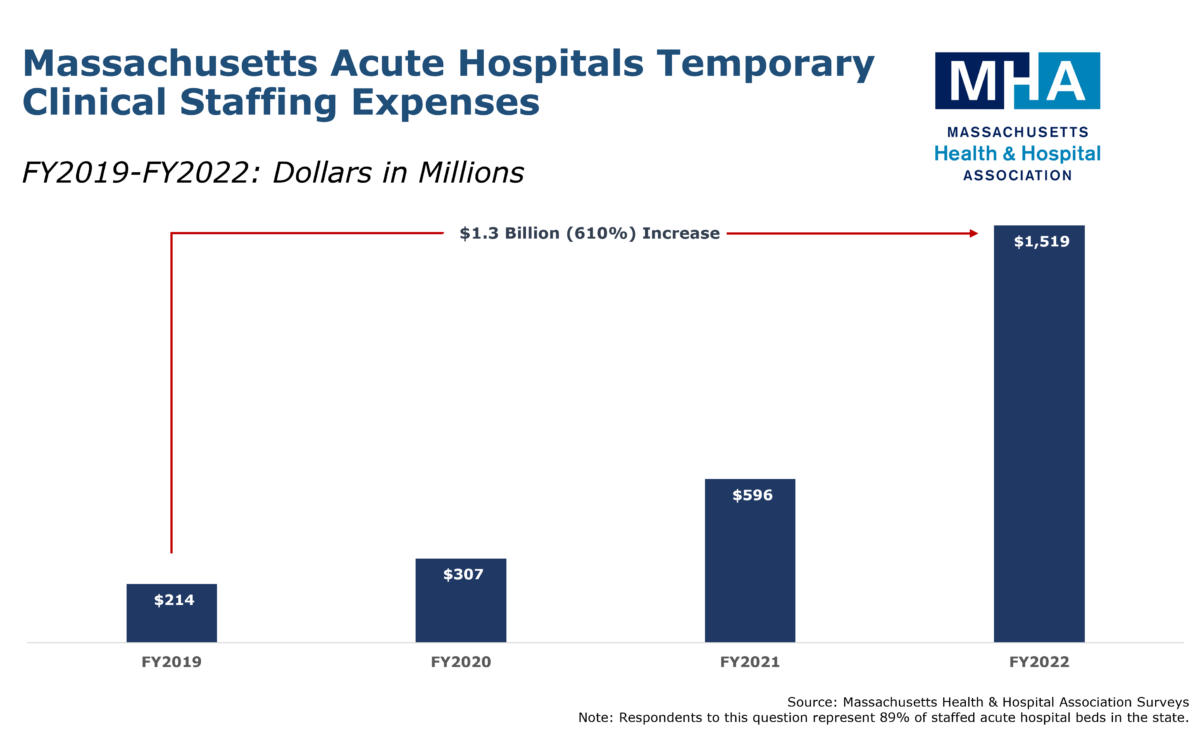
Hospital Temporary Labor Costs: A Staggering $1.52 Billion in FY2022
The COVID-19 pandemic disrupted the healthcare workforce market so dramatically that hospitals in 2022 spent $1.3 billion more for temporary staffing than they did pre-pandemic in 2019, according to an MHA survey of hospitals representing nearly 90% of staffed inpatient beds in Massachusetts.
To fill gaps in staffing, hospitals hire registered nurses and other staff through “traveler” agencies. Traveler workers, especially R.N.s in high demand, command higher hourly wages – at least two or three times more than what an on-staff clinician would earn. Many often receive signing bonuses. In Fiscal Year 2019, hospitals spent $204 million on temporary staff. In FY2022, they spent $1.52 billion – a 610% increase. According to the MHA survey, approximately 77% of the $1.52 billion went to hiring temporary R.N.s.
Labor accounts for close to 70% of a hospital’s operating costs. In addition to skyrocketing traveler agency costs, hospitals have increased average hourly wages for in-house staff from 13-to-20%, according to an MHA survey from late 2022. Hospitals are also offering extensive signing bonuses and retention packages to keep employees.
MHA conducted the survey to investigate and highlight the role of temporary labor on the overall financial instability still beleaguering the system.
“The healthcare workforce market in Massachusetts and around the U.S. has been upended and it is unclear where the change is taking us,” said MHA President & CEO Steve Walsh. “The traveler agencies and temporary-worker trend has introduced a highly volatile variable in the budgeting and forecasting models hospitals use to remain financially stable and accessible to patients. Any state effort to analyze and constrain healthcare cost growth must recognize this dramatic workforce shift now occurring. This is a trend that demands our collective policy focus.”
The Benchmark Misses the Mark
The state’s Healthcare Cost Growth Benchmark – a once-innovative model intended to cap healthcare costs in the state – has proven inadequate to assess the current state of the health system in the commonwealth, according to testimony MHA will submit to the Health Policy Commission (HPC) this Wednesday during the state’s annual cost-trend hearing.
MHA and its membership have repeatedly stated their commitment to cost control and the intended purpose of the benchmark. But the current system lacks a mechanism to assess in real time the $1.52 billion hospitals spent last fiscal year on temporary labor – a figure six times higher than what they spent pre-pandemic. The benchmark also has trouble accounting for how steadily spiking pharmaceutical costs, which hospitals cannot regulate, destabilize provider cost growth. And the benchmark process currently lacks the authority to prevent commercial health insurance companies from using the benchmark as a mechanism to squeeze rate concessions out of providers. Perhaps most notably, the benchmark was designed before the healthcare system, and the entire economy, faced input cost inflation of 7-to-8% annually.
“With the healthcare system still under heavy duress, the cost growth benchmark can only be a valuable tool if it is able to account for the new reality facing providers,” said Steve Walsh, MHA’s president & CEO and one of the architects of Chapter 224 during his time as chair of the House’s Health Care Finance Committee. “The cost pressures thrust upon hospitals and health systems within the past several years – particularly around temporary staffing – have simply become too pervasive to ignore. But these dynamics also represent a system that is undergoing fundamental change. It’s time that our approach to the benchmark follows suit and evolves along with every other part of the healthcare ecosystem. We look forward to our continued work with the HPC and partners across healthcare to keep access and cost at the forefront.”
ASPR Releases New Cybersecurity Guide for Healthcare Providers
Last Wednesday, the U.S. Department of Health and Human Services’ Administration for Strategic Preparedness and Response (ASPR) released a cybersecurity implementation guide to help healthcare organizations better manage their information technology system cyber risks. The guide includes risk management principles, best practices, and advice on organization structure to better prepare for cyber risks. Recent high-profile cyberattacks reinforce the need for companies and organizations to assess their cyber health and resilience and take actions to improve cybersecurity. Upgrading systems to protect from cyber attacks, which increased dramatically across the globe during the pandemic, is yet another rising cost for hospitals.
Hospitals, Insurers, SNFs Agree to Extend Transfer Plan
A voluntary plan to address the capacity crisis, first put into place in December 2022, has been extended another 45 days with some modifications, according to a memo released last week from the Executive Office of Health & Human Services.
The voluntary agreement between hospitals, commercial insurers, and nursing facilities in the state asks insurance companies to respond to hospital prior authorization requests within 24 hours for patient transfers from acute care hospitals to post-acute facilities, including weekends. This is a change from the prior flexibility that had insurers waiving prior authorization for post-acute care discharges. The nursing facilities under the plan agree to continue to extend admission hours through Saturday from 9 a.m. to 7 p.m., at a minimum, and to work to accommodate admissions 24/7. Hospitals agree to commence their discharge planning “as early in the day as possible.” The expedited transfer flexibilities will run for 45 days until April 20, 2023.
Health Insurance Companies Take Contrasting Prior Authorization Stances
Notably, Blue Cross Blue Shield of Massachusetts announced on March 8 that it will continue to waive prior authorization requirements for transfers from acute care hospitals – going beyond the requirements outlined in the EOHHS plan. This decision will assist skilled nursing facilities and acute rehabilitation hospitals manage the influx of inpatient admission requests. The Blue Cross flexibility will also remain in place until April 20, 2023.
However, another insurer, United Healthcare, has decided to not participate in the voluntary flexibilities to assist healthcare providers with their capacity constraints. United Healthcare has informed the state that it will not respond to hospital requests for prior authorization for post-acute care discharges within 24 hours, resulting in patients with United Healthcare insurance, who are ready for discharge, being unable to receive appropriate and timely rehabilitation and post-acute care services.
FOCUS ON WORKFORCE:
Building a Diverse Workforce Using the Tufts Medicine Dashboard

You can talk a lot about inclusion when building your workforce, but to really bring about changes you must build a roadmap to track your route to diversity and your progress in achieving it. That’s what Rosa Colon-Kolacko, the senior vice president and chief diversity, equity, and inclusion officer at Tufts Medicine, says in an interview included in MHA’s Workforce Toolkit.
“What culture do we have today? What culture do we want to have? What things do we have that are a plus?” Colon-Kolacko says are the questions organizations should ask. “And then map it out for a minimum of three years to see what path the journey will take as you connect it all – not only with data, but with education, learning programs, and more to make it part of the strategy of the organization.”
Colon-Kolacko says the roadmap process involves getting buy-in from all parts of the organization from the C-suite down to rank-and-file employees. Then the most important step is collecting data to ensure that an organization is using facts as it continues along its diversity path.
“We can say we’re struggling with retention, but where? In what population?,” she says. Data can show if applicants from certain populations are applying for jobs and where the facility’s focus needs to be. “We really want to make sure the dashboard is a mirror of outcomes and processes that can get us to a diverse workforce.”
Learn more about Tufts Medicine’s strategy, as well as about other workforce initiatives throughout the state, by visiting MHA’s Workforce Toolkit. Do you have a workforce program that you would like featured in the toolkit? Contact MHA’s Kim Stevenson at kstevenson@mhalink.org.
Biden’s Budget for FY24 Released
Last Thursday, President Biden released his fiscal year 2024 budget proposal. On the healthcare side, the budget proposes:
- extending the No Surprises Act to ground ambulances;
- permanently extending the enhanced Affordable Care Act tax credit;
- requiring private health plans to cover three behavioral health visits without cost-sharing, and requiring all plans to provide mental health and substance use disorder benefits;
- implementing a Medicare Advantage (MA) medical loss ratio requirement on MA supplemental benefits;
- significantly boosting Health Resources and Services Administration funding to aid “at risk of closure” rural hospitals and to aid rural healthcare workforce training programs; and
- expanding telehealth by boosting rural broadband.
Also last week the president released a brief outline of some of the Medicare reforms in the budget proposal, which he framed as steps to extend the financial viability of the Medicare Trust Fund. These Medicare savings proposals include raising the Medicare payroll tax on higher earners, eliminating payroll tax loopholes, and boosting the prescription drug reform savings by allowing more medications to have price negotiations after they come to market.
The release of the president’s budget kicks off the congressional budget season, which includes committee hearings and usually a budget resolution by early summer. Presidential budget proposals are traditionally more message documents than vehicles for action, but they often include ideas that Congress considers and can reflect issues which may be addressed in the federal rule-making cycle.
DEA Rules Would Restrict Use of Telehealth in Prescribing
The Drug Enforcement Administration (DEA) has released two proposed rules that would affect how controlled medications are dispensed through telemedicine. One rule would authorize practitioners to use telemedicine to prescribe a 30-day supply of non-narcotic Schedule III-V medications. To continue the prescription past 30-days would require an in-person examination with the prescribing practitioner. Schedule II controlled substances and narcotic Schedule III-V controlled substances would NOT be available to be prescribed via telemedicine and would require an in-person medical evaluation. The other rule would allow a 30-day initial buprenorphine prescription, but require an in-person visit before any additional prescriptions.
Last month, the Substance Abuse and Mental Health Services Administration (SAMHSA) also released proposed regulations that would limit the use of telemedicine to prescribe medication for opioid use treatment. MHA submitted a comment letter to SAMHSA outlining the barriers to access that the proposed regulations would cause. MHA is now reviewing the DEA proposals and intends to submit comments expressing concern that the proposed regulations will restrict access to telemedicine services and could be detrimental to patients needing buprenorphine and other medication treatment. These concerns are compounded by the ongoing burdens that healthcare facilities face with workforce, capacity, and throughput challenges.
Sen. Markey’s “Modernizing Opioid Treatment Access Act”
Senator Edward Markey (D-Mass.), chair of the Health, Education, Labor, and Pensions (HELP) Subcommittee on Primary Health and Retirement Security, joined by other members of Congress has filed the Modernizing Opioid Treatment Access Act.
The bill is intended to improve patients’ ability to access medication treatment for Opioid Use Disorder (OUD) by empowering board-certified physicians to prescribe methadone to patients and allowing U.S. pharmacies to dispense methadone.
While physicians can prescribe, and pharmacies can dispense, methadone for chronic pain, methadone for opioid use disorder is only available at Opioid Treatment Programs, which can be difficult to access for some people.
“In too many states across the country, every morning people have to travel for miles and miles to reach a clinic—if there’s one around at all—where they line up behind other patients waiting to get the medication they need,” Markey said. “If we want to beat these crises, we have to meet people where they are at with the resources they need. The Modernizing Opioid Treatment Access Act will reduce stigma and save lives.”
“Massachusetts hospitals and health systems are proud to support this legislation as they continue to use every resource in their reach to combat an intensifying opioid crisis,” said Leigh Simons Youmans, MHA’s senior director of Healthcare Policy. “This proposal would enhance that set of tools by helping providers reach patients where they are, and by expanding access to treatment that has saved countless lives to date. MHA applauds Senator Markey for his leadership on this critical issue.”
Transition
Executive Office of Health & Human Services Secretary Kate Walsh has appointed Audrey Morse Gasteier as executive director of the Massachusetts Health Connector. Morse Gasteier had been serving as acting executive director since January and has been employed by the Connector since 2012, most recently as director of policy and strategy. She holds an MS in Health Policy and Management from the Harvard T.H. Chan School of Public Health and a BA from Mount Holyoke College.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association 