Addressing the Capacity Crisis

INSIDE THE ISSUE
> Loan Repayment Program
> Pediatric Capacity
> Pediatric Plea to Biden
> Alternative Space Flexibility
> Ending the PHE
> Peer Support Network
> Therapeutic Guidance
> Funding to Fight Overdoses
MONDAY REPORT
Baker Administration Releases Critical, Targeted Workforce Funds
The Baker Administration last week addressed the healthcare workforce crisis by creating a $130 million loan repayment program for behavioral health and primary care workers.
Beginning in December, social workers, primary care physicians, psychiatrists, nurses, substance use recovery coaches, and case managers, among other care workers, can apply for funding to repay government or commercial loans. The program is targeted to workers in community health centers, community mental health centers, psychiatric units in acute care hospitals, in-patient psychiatric hospitals, or substance use treatment programs. Funding comes from the American Rescue Plan Act, which the legislature directed be used for this purpose, and the Opioid Recovery and Remediation Trust Fund.
The state said loan repayment awards will range between $12,500 and $300,000 per individual depending on their occupation, job setting, academic degree level, and whether the individual works part-time or full-time. Priority will be given to those who can communicate with patients in a language other than English, who work with historically medically underserved patients, who work in a designated Community Behavioral Health Center, and who work or reside in these communities that were prioritized in the COVID-19 Vaccine Equity Initiative: Boston, Brockton, Chelsea, Everett, Fall River, Fitchburg, Framingham, Haverhill, Holyoke, Lawrence, Leominster, Lowell, Lynn, Malden, Methuen, New Bedford, Randolph, Revere, Springfield, and Worcester. Information about how to apply will be made available by the Massachusetts League of Community Health Centers in December.
The unprecedented workforce shortages throughout the care continuum are straining the system. Patients cannot be transferred from one care setting to another because there are not enough workers to staff licensed beds. Backups occurring in facilities leads to “stuck” patients, behavioral health “boarding” in emergency department and other hospital units, and increased pressures on patients and staff.
“The pandemic has exacerbated workforce shortages across the healthcare and human services sector in both the public and private markets, placing significant stress on our healthcare providers, their staff and our Massachusetts residents seeking care,” said Health and Human Services Secretary Marylou Sudders. “Through this program, we are providing tangible support to sustain them in this high demand work.”
“Anything that helps to ease the tensions on our valued workforce and allows them to remain in their critical jobs is a win for patients and for the workers,” said MHA’s President & CEO Steve Walsh. “Hospitals are making the effort to recruit and retain workers through signing bonuses, career ladder incentives, scholarships for advanced learning, and their own loan assistance programs. We’re grateful that the Baker Administration and legislature have taken this profoundly important step to address the workforce crisis head on with critical funding.”
Resources and Helpline Help Counter Pediatric Capacity Issue
While the capacity crisis is affecting all parts of the healthcare system, pediatric capacity issues are currently of special concern throughout Massachusetts and the U.S.
Throughout the pandemic, children seemed to be more resilient against COVID-19 than other members of society. They were kept out of crowded classrooms, wore masks with less difficulty than others, and managed, comparatively so, to remain healthier than those who were older. Now, some clinicians believe, children are paying the price; they’ve returned to crowded classrooms, no longer wear masks, and are facing increasing number of infections because they have not built up immunity over the past three years.
As has been widely reported, inpatient pediatric care – especially care provided in pediatric intensive care units – is currently facing severe constraints in Massachusetts hospitals, due to the combination of workforce shortages and a dramatic increase in respiratory illness cases in children.
To counter the disturbing trend, Boston Children’s Hospital has set up a pediatric ICU consultative service for hospital peers. The 24/7/365 line assists in clinical management decisions and potential placement of patients. Also, the Regional Disaster Health Response System for New England has established a weekly webinar series through the end of the year to provide hospital clinical teams with information and resources to support their care of pediatric patients. Last week, MHA sent out guidance to its membership to access these services, and disseminated pediatric clinical protocols and other resources from Baystate Medical Center, Mass General Hospital for Children, and Boston Children’s, as well as from national hospitals.
Pediatric Hospitalizations a National “Emergency”
The pediatric capacity problem is not specific to Massachusetts. The rise in pediatric respiratory syncytial virus (RSV) and influenza, along with an increase in childhood mental health cases, has reached the level of a “national emergency,” according to a letter the Children’s Hospital Association and American Academy of Pediatrics sent last week to President Joe Biden and U.S. Health & Human Services Secretary Xavier Becerra.
“Across the country, more than three-quarters of pediatric hospital beds are full, and many states are reporting more than 90 percent of their pediatric beds are occupied,” the groups wrote. “This is mirrored in community settings, where ambulatory pediatric practices are facing tremendous demand and workforce shortages … We are particularly concerned that historically under-resourced communities will be disproportionately impacted. The pediatric healthcare system is doing all it can to meet these overwhelming needs across the continuum of care and taking regional approaches to meet the growing demands. We need emergency funding support and flexibilities along the same lines of what was provided to respond to COVID surges.”
In the letter, the groups outline a series of steps the federal government could take if the president issued “a declaration of an emergency under the Stafford Act or National Emergencies Act and a Public Health Emergency declaration.”
Capacity Crunch Leads to State Extending Alternative Space Flexibility
State and federal flexibilities issued during the height of the pandemic allowed hospitals to use alternate spaces within their facilities for inpatient care. Last week, the Department of Public Health at the urging of hospitals extended the alternate space flexibility through however long the federal COVID-19 “blanket waiver” for healthcare facilities lasts (see related story below) – and added special conditions for pediatric patients.
“DPH will continue to permit DPH licensed or operated hospitals to use alternate acute inpatient care space to care for adult medical/surgical service inpatients and adult medical/surgical service patients awaiting admission, and now allow these facilities to use this space to care for pediatric medical/surgical service inpatients and pediatric medical/surgical service patients awaiting admission,” the department wrote. “… The purpose of this memorandum is to continue to enable hospitals to increase the number of patients cared for by providing additional or alternate space to meet the demand and ongoing infection control best practices given the ongoing high levels of community transmission of COVID-19 and demand for healthcare system utilization.”
The seven-page DPH memo outlines the strict guidelines and limitations hospitals must follow when using alternate spaces.
So When Will the National Public Health Emergency End?
Every 90 days since the national COVID-19 Public Health Emergency (PHE) was first declared in January 2020, the federal government has renewed the declaration. And with each renewal, officials have said they will give 60-day notice in the event the declaration is not renewed.
The current 90-day PHE declaration is set to expire in January 2023, meaning that the 60-day notice of its potential revocation would have been on November 11. But that notice was not given. Reuters quoted two unnamed administration officials on that day who indicated the PHE would be extended again in recognition of the expected winter surge in COVID cases, and the difficulty in transitioning vaccines and treatments from government control to the private sector.
New Virtual Peer Support Network from the Betsy Lehman Center
Many Massachusetts hospitals offer peer support within their walls but some healthcare workers do not have access to an onsite program. Now, free, confidential 1:1 peer support is available for anyone in Massachusetts whose work relates to patient care. The Virtual Peer Support Network matches health workers to colleagues across the state who are trained to help with the pressures that can accompany working on the front lines of care.
Individuals can seek help by completing this request form or calling (617) 701-8101. Those interested in being trained as a peer supporter can fill out this volunteer form. Organizations that would like to promote the network in their workplaces as a new resource for employees can e-mail Jacqueline.Ewuoso@BetsyLehmanCenterMA.gov.
As COVID Changes in Mass., So Does Recommended Treatment
The COVID-19 variants affecting Massachusetts are shown in the CDC’s Nowcast weekly posting. DPH, after reviewing the latest posting on November 11 sent notice to providers telling them that one therapeutic tool – bebtelovimab – should no longer be used because it is not effective against 40% of the variants prevalent in the state.
Bebtelovimab therapy had been used to treat COVID-19 in individuals for whom the main preferred treatment – Paxlovid – is not clinically appropriate. Now that bebtelovimab is unlikely to be effective, clinicians should use Remdesivir if the patient can’t accept Paxlovid. Paxlovid is a series of pills taken over 5 days; remdesivir is administered through three daily intravenous infusions. Paxlovid and remdesivir are readily available in Massachusetts, DPH says in this therapeutic guidance document. Getting vaccinated and receiving the proper therapeutic when needed is the best way to keep people out of the hospital and assist in easing the capacity crunch now destabilizing the healthcare system.
RIZE Provides Grants to Fight Overdoses
RIZE Massachusetts – the independent, non-profit working to end the overdose scourge – last week awarded $100,000 grants to six community-driven projects, including ones for the Grayken Center for Addiction at Boston Medical Center and the Grayken Center for Treatment at South Shore Health.
The BMC Greyken Center will use the funding to enhance a 24/7 overdose prevention hotline staffed by peers with lived experience by using “virtual spotting” remote technology that prompts a rescue response if an overdose occurs. South Shore Health Greyken Center’s grant will go to increase hospital initiation of methadone, along with peers following up with patients to ensure early retention in the program when the risk of dropout is high. Read about all the recipients’ programs here.
Happy Thanksgiving!
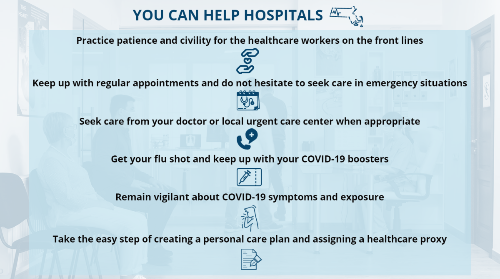
Monday Report is taking a brief break over the holiday and will return on Monday, December 5. MHA extends its thanks this holiday season to all of the healthcare professionals who dedicate themselves to keeping individuals, families, and communities safe and healthy. The best way for us to truly thank caregivers is to take basic steps of keeping ourselves healthy, getting care in the right place at the right time, and treating the people who care for us with the respect they deserve.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association