Advancing Hospital to Home; Phase 2 of Redeterminations

INSIDE THE ISSUE
> Gov. Funds Hospital at Home
> Phase 2 of Redetermination
> Mobile Integrated Health
> FOCUS ON WORKFORCE: Baystate Health
> SUD Program Funding
> ACCESS Act Resources, Course
> Independent Dispute Resolution
> April Programs: ACHE and Betsy Lehman Center
MONDAY REPORT
Healey Moves to Bolster Hospital to Home Program
The so-called “throughput” problem – that is, the difficulty moving patients out of an acute care hospital to a skilled nursing facility (SNF) or other post-acute care setting – has many causes. From insurance prior authorizations and administrative delays to workforce vacancies in the non-acute settings, the roadblocks to transfers result in patients not receiving the care they need when they need it, and acute care hospital beds being filled by patients who no longer require that level of care. As many as 1,000 patients that do not require acute care are regularly “stuck” in Massachusetts hospitals as they await a transfer to occur.
Last week, the Healey Administration took an additional step to mitigate the crisis by awarding $3 million in grants to acute care hospitals and Aging Services Access Points (ASAPs) across Massachusetts through the Hospital to Home Partnership Program. Hospitals and ASAPs work together to enable hospital patients to transition directly to home and community-based settings after discharge, with appropriate services and supports.
ASAP awardees will use the funds to hire personnel who work with the hospital and other regional partners. Awardees may also use the funds to implement programs or technologies that will ease patient transitions from hospital to home.
The awardees are:
- Greater Springfield Senior Services in partnership with Baystate Health
- Western Mass Eldercare Inc. in partnership with Holyoke Medical Center
- Elder Services of Worcester in partnership with UMass Memorial Health
- Tri-Valley Inc. in partnership with Milford Regional Medical Center
- AgeSpan Inc. in partnership with Lawrence General Hospital
- Somerville Cambridge Elder Services in partnership with Cambridge Health Alliance
- Mystic Valley Elder Services Inc. in partnership with Tufts Medicine Melrose Wakefield Hospital
- Springwell Inc. in partnership with Newton Wellesley Hospital
- Old Colony Elder Services In. in partnership with Beth Israel Deaconess – Plymouth
“MHA and our members are deeply grateful for the Healey-Driscoll administration’s investment in community-based care at a time when it is needed most,” said MHA President & CEO Steve Walsh. “In addition to providing individuals with the supports they need after leaving the hospital, this program will help open beds for other patients who require an acute level of care. Our healthcare system remains under significant pressure, and this is a solution that can make a tremendous difference for care access, wait times, and the strain on caregivers.”
The Hospital to Home Partnership is a $3 million pilot for which a host of hospitals applied to participate. Funding for the grant came from the American Rescue Plan Act and provides up to $300,000 to awardee ASAPs and hospitals in partnership over the next two years. MHA has also asked for additional funding for the program in the FY24 budget since there is additional demand from hospitals to work with their ASAP partners.
MassHealth Redeterminations: Keep an Eye Out for The Blue Envelope
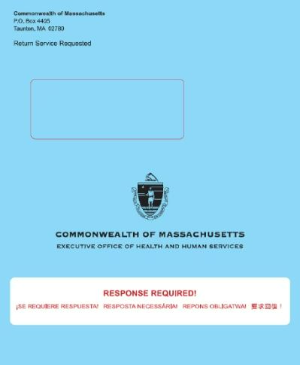
Phase 2 of the MassHealth redetermination process began last week in anticipation of this Saturday’s – April 1 – formal start of the year-long initiative to renew all MassHealth members.
Advocates, including the provider community, will be working with MassHealth members to remind them of the need to re-apply. The main messages MassHealth wants to get across to its members during Phase 2 are:
Update your information. Make sure MassHealth has your most up to date address, phone number, and e-mail so you do not miss important information and notices from MassHealth.
Read all your mail. MassHealth will be sending renewal form in a blue envelope. Additional important notices or request for information may arrive in white envelopes.
Respond to MassHealth before the deadline. The notice enrollees receive will have a deadline and all forms must be sent by that deadline.
MHA Endorses Legislation to Advance Mobile Integrated Health
Mobile Integrated Health (MIH) is the practice of using paramedics, in coordination with healthcare facilities and other providers, to deliver care services to patients who are not facing a dire emergency.
These MIH programs, reviewed and approved by the Department of Public Health, ensure that patients receive appropriate care services while minimizing hospital readmissions and unnecessary visits to emergency departments. However, providers have been hesitant at times to invest in the resources necessary to establish MIH programs because there is no guarantee that public and private health insurers will provide the reimbursement needed to sustain them.
For the last several legislative sessions MHA has filed An Act Relative to Insurance Coverage of Mobile Integrated Health, which this session is numbered H.1007/S.718, and was filed by Rep. Michael Finn (D-West Springfield) and Sen. Walter Timilty (D-Milton). The bill would prevent public and private health plans from refusing to cover healthcare services on the basis that they were delivered by a state-approved MIH program. It would also require MIH services to be covered to the same extent as they would have had they been provided in a healthcare facility.
The MHA-endorsed bill would also lift application and registration fees for MIH programs that are focused on delivering behavioral health services. As shown by MHA’s weekly survey (see below), hundreds of children and adults, many with increasingly acute psychiatric needs, now board in hospital emergency departments and med-surg units. MIH can support these behavioral health patients while simultaneously reducing emergency department boarding.
South Shore Health has an MIH program that proved invaluable during the pandemic by allowing chronic patients to receive care at home, which prevented unnecessary hospitalizations and controlled the spread of COVID-19. The program provided mobile COVID-19 tests and vaccinations, treated patients with mild COVID-19 symptoms, and even participated in a Remdesivir clinical trial. These services are in addition to treating patients in their homes for acute and chronic health issues, such as congestive heart failure, chronic obstructive pulmonary disease (COPD), pneumonia, cellulitis, dehydration, and behavioral health conditions. However, with no reimbursement from health plans for MIH services, the program – which is currently funded by public donations and agreements with community groups – is therefore at risk.
FOCUS ON WORKFORCE:
Baystate Health: Strategic Collaboration to Grow the Workforce

In this installment of our weekly focus on what Massachusetts providers are doing to grow the healthcare workforce during a period of troubling vacancies across the system, Baystate Health’s Patricia Samra, VP of HR Operations and Total Rewards, and Jason Pacheco, director of Workforce Planning, Analytics, and Compensation at Baystate describe how the system’s three-year strategic workforce planning process informs their efforts to attract, train, and retain workers.
Baystate is part of the Western Mass. Healthcare Collaborative that has two arms – the Western Mass. Nursing Collaborative and another entity covering all other healthcare workforce positions.
Originally grant funded, the collaboratives – consisting of area providers, schools, and other groups with a common goal of breaking down barriers and providing opportunities for employment – are now funded through dues from each participating organization.
Baystate develops dual pipelines, focusing on “outside-in” and “inside-up” strategies to train and promote staff.
Learn more about Baystate Health’s program, as well as about other workforce initiatives throughout the state, by visiting MHA’s Workforce Toolkit. Do you have a workforce program that you would like featured in the toolkit? Contact MHA’s Kim Stevenson at kstevenson@mhalink.org.
Funding Available for Hospital-Based Substance Use Disorder Programs
Up to $7 million annually, or a total of $63 million over the nine-year course of a new state initiative is available to hospitals that can create hospital-based addiction and substance use disorder treatments that will increase access to patients presenting to the emergency department or admitted to inpatient level of care. Potential models that will be funded include, but are not limited to, hospital addiction care teams and/or bridge clinics that are co- or closely located to a hospital ED. Programs that use telehealth approaches for coverage will also be accepted.
The overall goals of this Request for Responses from DPH’s Bureau of Substance Addiction Services (BSAS) are to increase access to hospital-based services, ensure ongoing linkages to care and community-based follow-up, promote wellness and long-term recovery, and, most importantly, reduce overdose deaths. The RFR is the latest initiative stemming from DPH’s and BSAS’s collaboration with MHA and its member hospitals.
The RFR is due back to DPH by April 24 at 4 p.m. A bidder’s conference will be held on April 5, at 3:15 p.m. Details are in the RFR link above.
ACCESS Law: Free Course and Materials
An effort is underway to better educate consumers, pharmacists, and providers about the Massachusetts ACCESS Law, under which eligible people can get a year’s supply of prescription birth control at no cost with one trip to the pharmacy. The law covers a year’s supply of the pill, patches, rings, or injectable birth control, but does not cover male condoms and vasectomies, or contraception that last for extended periods, such as IUDs or implantable rods.
There is a new online course that explores the provisions and limitations of ACCESS (An Act Relative to Advancing Contraceptive Coverage and Economic Security in Our State, passed in 2017). The course is for Massachusetts physicians, nurse practitioners, and physician associates and includes information about the new statewide standing order for emergency contraception pills. Attendees can earn 2.5 continuing education credits at no cost; the Department of Public Health covers the cost of the course which was created with the MGH Institute of Health Professions.
Also, there is a host of public messaging materials that MHA members can share on their channels or distribute in facilities. MHA has collected the materials from DPH here.
New Rules for No Surprises Act’s IDR Process
Independent dispute resolution (IDR), the process whereby an independent arbiter resolves payment disputes between providers and insurers under the “No Surprises Act,” are back underway with new guidance from the federal government.
The IDRs were on hold while a court case in Texas challenged the metrics used to determine the payments. Providers won the court case that found that the rules the federal government issued relied too much on the Qualifying Payment Amount (in essence, a health insurer’s median contracted rate) which unfairly shifted the arbitration in favor of the insurers. During the court case certain IDRs were halted.
The Centers for Medicare and Medicaid Services (CMS) recently instructed IDRs to resume and it issued this guidance document outlining the new process for arbitration. Observers note that in the new regulations CMS has carefully skirted the QPA issue, signaling a temporary win for providers; however, it is unclear if the issues brought up in the Texas court case will continue through the appeal process.
Mark Your Calendars for These Two April Programs
Tuesday, April 25, 8 a.m. to 12:30 p.m. – ACHE of MA’s Spring Forum: The Evolving Healthcare Landscape –Perspectives from Today’s Industry Leaders and Visionaries. Click here to register.
This forum at Waltham Woods Conference Center features, among other presentations, a panel with Jessica Dudley, M.D., the chief clinical officer at Press Ganey; Heather Trafton, president & CEO, Mass Advantage; and Charlie Buck, a partner with McDermott, Will & Emery; moderated by Andy Shin, SVP Strategy, Mass General Brigham.
David Rendall, author of The Freak Factor: Discovering Uniqueness by Flaunting Weakness, will deliver the keynote address.
Wednesday, April 26, 8 to 11:30 a.m. – Mass. Health Policy Forum/Betsy Lehman Center: Roadmap to Healthcare Safety for Massachusetts. Click here to register.
The Roadmap to Healthcare Safety for Massachusetts sets five patient safety goals across the care continuum and introduces a set of strategies and action steps for achieving them through a phased, multi-stakeholder approach. It was produced by the Massachusetts Healthcare Safety and Quality Consortium, which is a collaboration of the state’s policymakers, providers, payers, and patient advocates led by the Betsy Lehman Center for Patient Safety. MHA is an active member of the consortium and played a role in producing the Roadmap. The forum is free and will be held at the Omni Parker House in Boston.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association