Behavioral Health Bill, SCOTUS on 340B, and more…

INSIDE THE ISSUE
> Mental Health Bill
> Supreme Court Ruling on 340B
> July 1 Sequester Cut
> Health Plan Profits
> The Nurse Licensure Compact
> Mass. Considered National Health Leader
> Vaccine Communication
> Juneteenth
MONDAY REPORT
Massachusetts House Passes Mental Health Bill
The Massachusetts House of Representatives unanimously passed a bill last Thursday aimed at improving the state’s behavioral health system.
Much of H.4879, An Act Addressing Barriers to Care for Mental Health, focuses on a more collaborative approach to addressing the state’s behavioral health crisis by teaming providers and payers together to more efficiently and fairly meet the needs of some of the most at-risk patients. For example, the House bill requires health plan coverage of mental health acute treatment, community-based acute treatment, and intensive community-based acute treatment without prior authorization. It also enhances oversight of health plans for mental health parity compliance, mandates that commercial plans cover emergency services programs (ESPs), and requires coverage of annual mental health wellness exams. The wellness exams, as well as many other provisions in the House bill are contained in a behavioral health Senate bill passed last November. The two chambers will now meet in conference to craft a bill that can be sent to the governor’s desk.
The House adopted an MHA priority amendment, filed by Representative Marjorie Decker (D-Cambridge), that requires commercial health plans, MassHealth, and Group Insurance Commission health plans to provide reimbursement for each day that a patient boards in an emergency department, on a medical surgical floor, or in an observation unit for behavioral health admission. Given the current boarding environment, MHA and its partners in the behavioral health field have long argued that reimbursement for behavioral health boarding is critical to ensure patient care and workforce needs are met.
“This legislation is another stride toward achieving effective mental health coverage in the commonwealth,” said Leigh Simons Youmans, MHA’s senior director of healthcare policy. “Meaningful parity and reimbursement improvements like these can help alleviate virtually every challenge that the behavioral health system is facing – including workforce shortages and bed availability. We are especially grateful for the passage of an amendment that will ensure hospitals are provided with the resources they need to best care for the more than 600 behavioral health patients boarding in their facilities. This measure — made possible by the leadership of Speaker Mariano, Representative Madaro, and Representative Decker – is a tremendous step forward as we confront the boarding crisis one day and one patient at a time.”
Supreme Court Rejects U.S. HHS Rule on 340B Drug Costs
U.S. Health & Human Services (HHS) did not follow its own procedures when it cut reimbursement rates for hospitals within the 340B prescription drug program that serve low-income populations, the U.S. Supreme Court ruled unanimously last week. As such the $1.6 billion in cuts have been overturned.
At issue is an interpretation of the Medicare statute that gives HHS two options for setting reimbursement rates for certain outpatient prescription drugs. Under Option 1, HHS conducts a survey of hospitals’ acquisition costs for each covered outpatient drug and then can set rates based on the hospitals’ “average acquisition cost” for each drug, and then can vary the rates “by hospital group.” If it doesn’t conduct a survey first, HHS can set reimbursement rates based on “the average price” charged by manufacturers for the drug as “calculated and adjusted by the Secretary.”
Option 2 does not authorize HHS to vary reimbursement rates for different hospital groups, but that is exactly what it did in 2018 and 2019; it didn’t conduct a survey, but it cut rates for a specific group of hospitals – the 340Bs.
“For 2018 and 2019, HHS did not conduct a survey of hospitals’ acquisition costs for outpatient prescription drugs,” Associate Justice Brett Kavanaugh wrote. “But HHS nonetheless substantially reduced the reimbursement rates for one group of hospitals—Section 340B hospitals, which generally serve low-income or rural communities. For those 340B hospitals, this case has immense economic consequences, about $1.6 billion annually.”
The American Hospital Association brought suit against HHS. MHA joined other hospital interests in filing an amicus brief on the case. AHA is now working with the Biden administration to determine how and when the 340B hospitals that were harmed by the cuts in 2018 and 2019 can receive reimbursement for their losses.
Looming Sequester Cut Threatens Hospitals
The federal omnibus spending bill signed into law in March that kept the government operating failed to rescind, to the dismay of hospitals, the 1% across-the-board Medicare payment cut scheduled to go into effect on July 1.
A 1% Medicare sequester cut took effect April 1 and will increase to 2% on July 1 if Congress does not act.
In a letter to Congressional leaders last week, the American Hospital Association detailed the steady pressure on hospitals, rising input costs – including spiraling workforce costs – and the static nature of hospital prices.
“Unlike other sectors of the economy, hospitals and health systems cannot deflect these increased costs,” the AHA wrote. “A majority of payments to hospitals and health systems are dependent on Medicare and Medicaid — which reimburse hospitals less than the cost of providing care and are non-negotiable, fixed reimbursement rates. These fixed costs don’t allow hospitals to absorb or deflect the impact of the historic inflation levels. In fact, 94% of hospitals have 50% or more of their inpatient days paid by Medicare or Medicaid, and more than three quarters of hospitals have 67% or more Medicare or Medicaid inpatient days.” The AHA projected that hospitals will lose at least $3 billion by the end of the year.
MHA Releases Semi-Annual Health Plan Performance Report
MHA is releasing its Semi-Annual Health Plan Performance Report which presents an analysis of the financial position of health plans in Massachusetts from January 2017 through December 2021, with a focus on 2021. The report details how the COVID-19 pandemic resulted in unprecedented profits and surplus for many health insurers. Massachusetts health plans now collectively report statutory net worth surpluses that exceed $6.1 billion in the aggregate, which represents a 22% increase during the pandemic years and a 58% increase since 2015. The amount of net worth surplus that exceeds 500% of risk-based capital (RBC) for all plans was $1.12 billion in 2021. Four health plans are either closely approaching or exceeding 600% RBC: HMO Blue, Harvard Pilgrim Health Care, Tufts Health Plan, and United Healthcare of New England. RBC is a measure of financial solvency; a health plan may be subject to Division of Insurance intervention whenever its RBC ratio falls below 200%.
MHA produces the report to keep member hospitals, health systems, and PHOs up to date on trends in financial performance and membership among the most prominent health plans in the market.
The Nurse Licensure Compact
With the end of the state’s legislative session ticking closer, a broad coalition of those within the healthcare community are hopeful that the Nurse Licensure Compact (NLC) will be among the proposals that pass by the session’s July 31 deadline.
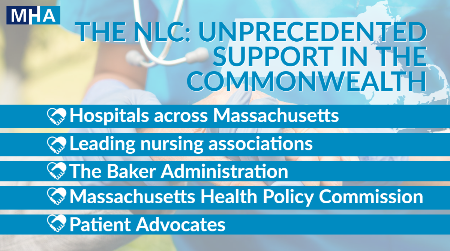
The NLC allows Massachusetts to join 39 other states in a joint licensing agreement that permits nurses to have one multistate license from the state in which they reside, with the privilege to practice in their home state and all others that are members of the Compact. MHA, nursing groups, other provider organizations, the Baker Administration, many legislators, and the Health Policy Commission – among others – have long supported the commonwealth’s entry into the Compact.
Compact nurses can “follow” their patients across state lines and continue to provide care and counseling through telehealth. During flu season and public health emergencies, Compact nurses can easily cross state lines to fill vacancies in other states. In short, the Compact is an efficient, proven way to address a part of the workforce dilemma that is reverberating throughout the entire healthcare system.
The Health Policy Commission in May 2021 issued a report endorsing the NLC, saying it would help Massachusetts “react more dynamically to unforeseen and sudden changes in nursing needs, during pandemics and other emergencies.”
“Amid the difficult policy choices and complexities facing the health care system, the Nurse Licensure Compact presents a ‘low-hanging-fruit,’ easily obtainable solution that would go far in assisting caregivers and their patients at a time when qualified caregivers are at a premium,” said MHA President & CEO Steve Walsh. “We urge legislators to help make us the fortieth compact state by sending an NLC bill to Governor Baker this session.”
Mass. Leads Nation in Many Health Measures
The private foundation – The Commonwealth Fund – has released its 2022 scorecard on state health system performance, and Hawaii and Massachusetts ranked as Number 1 and 2, respectively. The rankings are based on overall performance across 56 measures of healthcare access and quality, service use and cost, health disparities, and health outcomes during the COVID-19 pandemic in 2020.
Massachusetts led the nation in the following categories: Access & Affordability, Prevention & Treatment, Healthy Lives, and Racial & Ethnic Equity. It was second in Income Disparity and in a new special category that assessed the state’s performance using eight COVID-19-specific measures, the commonwealth ranked eight nationally.
Free Vaccine Communication Training for Providers
In partnership with the Department of Public Health and the Center for Integrated Primary Care at UMass Chan Medical School, the Perinatal-Neonatal Quality Improvement Network of MA (PNQIN), of which MHA is a member, created a Communication Skills Training for Clinicians Discussing COVID-19 Vaccination. The motivational interviewing concepts and skills covered are applicable to all types of vaccination and other health decisions. The asynchronous training recording is available here. Free continuing education credits (CME, CEU, and Social Work) are available to Massachusetts providers.t.
Happy Juneteenth

MHA offices are closed today in celebration of the National Juneteenth holiday. The day commemorates the June 19, 1865, General Order #3 by Major-General Gordon Granger of the Union Army in Texas, who wrote: “The people of Texas are informed that, in accordance with a proclamation from the Executive of the United States, all slaves are free. This involves an absolute equality of personal rights and rights of property between former masters and slaves, and the connection heretofore existing between them becomes that of employer and hired labor.”
In recent years, MHA has redoubled its efforts to become a more equitable workplace and to use its influence to press for change across the commonwealth. In addition to creating a board-level Standing Committee on Diversity, Health Equity & Inclusion (DHE&I), and hiring a Director of Health Equity, MHA has an internal Staff Council on Diversity, Equity, and Inclusion to ensure an inclusive workplace and spark conversations that foster a deeper understanding of DHE&I topics. MHA is committed to weaving diversity, equity, and inclusion into the fabric of our work and the work of the entire healthcare community. As an advocacy organization, it is especially crucial that MHA brings a DHE&I lens to policy and legislation, as well as to its work with state agencies and other stakeholders.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association