INSIDE THE ISSUE
> The House Budget & Amendments
> National Data Confirms Mass. Data
> No New Flexibilities
> COVID-19 Vaccine Update
> Lehman Center’s Roadmap to Safety
> Executive Insight Series: Seltz
> AHA Podcast: MHA’s Code of Conduct
> In Memoriam
MONDAY REPORT
House Budget Debate Begins Today
Debate on the Massachusetts House’s Fiscal Year 2024 state budget is scheduled to begin today. On April 12, the House’s Ways & Means Committee released its $56.2 billion spending plan and by April 15, more than 1,500 amendments to the budget had been filed. Among those amendments are 19 that MHA and the healthcare community consider priorities, including amendments relating to improving the behavioral health system, building the healthcare workforce, helping to alleviate the capacity crunch, strengthening telehealth, and continuing enhanced Medicaid payments to eligible hospitals.
“The legislature has been responsive throughout the pandemic in taking vital steps to assist our healthcare system,” said MHA President & CEO Steve Walsh. “To fully meet the needs of patients and communities as we come out of the pandemic, healthcare organizations and the people they employ will need continued support.”
For example, a key set of amendments sponsored by Rep. Marjorie Decker (D-Cambridge) would strengthen the Mental Health Addressing Barriers to Care Act, or ABC Act. Amendment 728 would address workforce challenges and behavioral health access by codifying regulations the Department of Public Health promulgated that expand the definition of licensed mental health professionals to include certain master’s level clinicians working towards licensure. The ABC Act required insurers to cover services provided by individuals with a master’s degree if that clinician was working in an outpatient clinic. Amendment 728 would extend that requirement to similarly trained clinicians in acute care hospitals. Amendment 731 brings some provisions of the ABC Act in line with reforms made under the Roadmap for Behavioral Health Reform, which was implemented after the ABC Act. Specifically, 731 ensures insurance coverage when hospitals provide ED-based behavioral health crisis evaluations, which were previously provided by Emergency Services Programs. Among five priority workforce amendments, Amendment 1085 filed by Rep. Lindsay Sabadosa (D-Northampton) would create a pipeline program between hospitals and colleges to train and employ interested students in mental health worker positions.
Hospitals Face “Existential Challenge”
A new report from the American Hospital Association (AHA) outlines how U.S. hospitals are facing “an existential challenge — sustained and significant increases in the costs required to care for their patients and communities.”
The AHA report confirms the research that MHA has conducted over the past months demonstrating that Massachusetts hospitals are facing unprecedented labor shortages, contract labor expenses that exceeded $1.5 billion in 2022, capacity constraints, and financial shortfalls.
AHA’s report demonstrates that the increase in expenses for drugs, supplies, and labor, as well as the costs associated with administrative burden, have been met with continued underpayments from government payers. “In fact, the growth in hospital expenses is more than double the increases in Medicare reimbursement for hospital care,” AHA reported, resulting in more than half of U.S. hospitals ending 2022 operating at a financial loss.
In Massachusetts, a report this month from the Center for Health Information and Analysis (CHIA) showed that 70% of health systems in the commonwealth had negative operating margins during the most recent quarter of Fiscal Year 2023. The statewide median operating margin for acute hospitals during that quarter (ending December 31, 2022) was 0.9%, a decrease of 0.5 percentage points compared to the same period in the prior year, CHIA’s report shows.
AHA’s national cost report shows that the median price of a new drug exceeded $200,000 in 2022 or “more than triple the median annual household income in the U.S.” At the same time, price increases for existing drugs continue to outpace inflation. AHA’s data shows that hospital supply expenses per patient increased 18.5% between 2019 and 2022, outpacing increases in inflation by nearly 30%. “Purchased service expenses” – that is, operational efficiency expenses relating to IT, environmental services, food and nutrition, among other costs – increased 18% between 2019 and 2022. And, AHA noted, “the burden associated with insurer-required administrative tasks also contributes to rising expenses and negatively affects patient care. Nearly three-fourths of nurses reported increases in insurer-required administrative tasks for medical services over the last five years. In addition, nearly 9 in 10 nurses reported insurer administrative burden had negatively impacted patient clinical outcomes.”
CMS: No New COVID-19 Waiver Requests!
As has been well reported, the U.S. healthcare system was able to survive the pandemic in part because the federal government instituted a series of waivers and flexibilities to ease regulatory burdens. The Centers for Medicare and Medicaid Services (CMS) instituted many of those so-called “1135 waivers” (named for the relevant section of the Social Security Act). Last week CMS sent notice that it is no longer accepting any new 1135 waiver requests. The agency once again urged providers to “begin reestablishing previous health and safety standards and billing practices.”
MHA continues to work with its members and federal partners to prepare for the most significant changes that will come with the end of the public health emergency on Mary 11.
Clarification on COVID-19 Vaccines
The Food and Drug Administration last week issued up-to-date guidance on COVID-19 vaccines. The main takeaway is that the monovalent versions of the Pfizer and Moderna vaccines – that is, the two-shot regimen that was prevalent during the start of the vaccination program – are no longer authorized.
People aged 65 and over, who have already received a bivalent shot, should get an additional bivalent booster at least four months after their initial dose, the FDA says. That’s because evidence shows waning vaccine immunity in this population, according to the agency. The same is true for immunocompromised individuals; they should get a bivalent booster shot. The FDA notice also provides information relating to vaccine updates for children.
But what about the rest of the population, aged 18 to 65, who have been vaccinated and boosted with a bivalent vaccine? The FDA says they are not eligible for another bivalent shot now. In June, however, the FDA’s Vaccines and Related Biological Products Advisory Committee will hold a meeting to discuss vaccine strains going forward. “Much like the FDA does yearly with the influenza vaccines, the agency will seek input from the committee on which SARS-CoV-2 variants and lineages are most likely to circulate in the upcoming year,” the FDA wrote. “Once the specific strains are selected for the COVID-19 vaccines, the FDA expects manufacturers to make updated formulations of the vaccines for availability this fall.”
This Wednesday: Major Healthcare Safety Program
A Roadmap to Health Care Safety for Massachusetts will be released this Wednesday, April 26 at a live event hosted by the Massachusetts Health Policy Forum. The Roadmap sets a bold aim, calling for actions to propel big gains in safety across the continuum of care. It was produced by the Massachusetts Healthcare Safety and Quality Consortium, a sustained collaboration of the state’s policymakers, providers, payers, and patient advocates led by the Betsy Lehman Center for Patient Safety. Learn more and register here for this free event at the Omni Parker House in Boston.
A Conversation with the HPC’s David Seltz
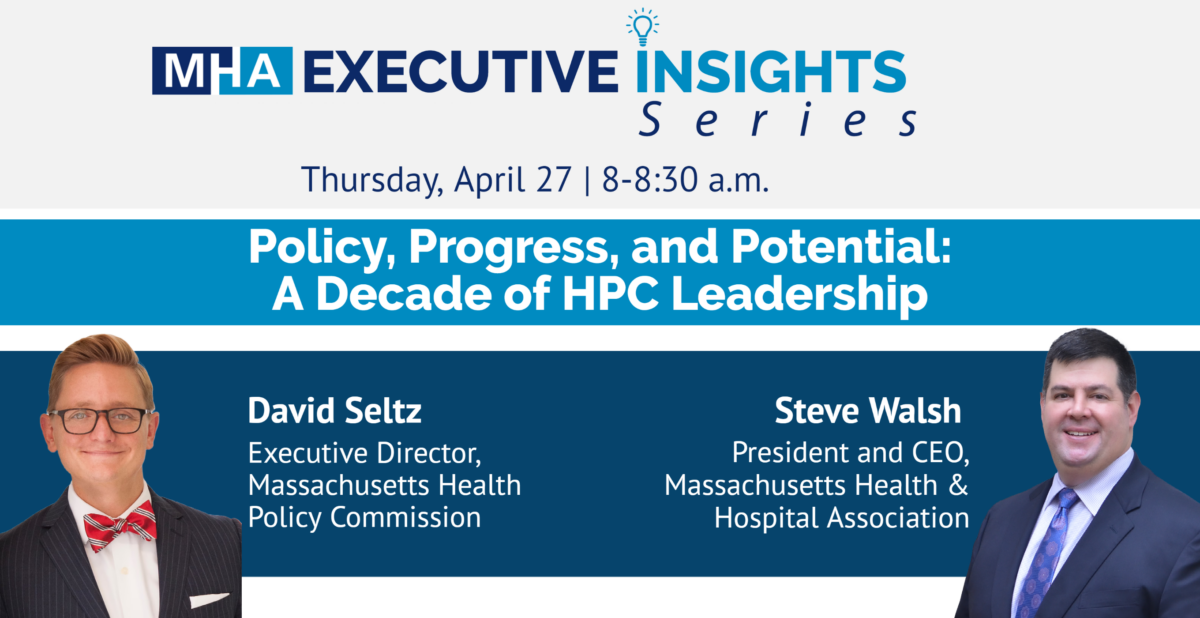
MHA’s popular Executive Insights series makes a return this Thursday.
The series has featured up-close interviews with nearly a dozen healthcare CEOs since its launch in 2021. Now, MHA is stepping outside of its membership to feature a free-flowing conversation with David Seltz, Executive Director of the Massachusetts Health Policy Commission. Seltz has overseen the HPC since its inception just over a decade ago, and has helped drive discussions around healthcare reform, cost strategies, and innovation. He will join MHA’s Steve Walsh to talk about his background, his take on current healthcare challenges, and his vision for the future of the system. Register for the free event here.
MHA’s Anti-Violence Code of Conduct is Focus of National Podcast
A January 2023 MHA report on healthcare violence and the resultant Code of Conduct from the MHA Board of Trustees was the focus of a podcast from the American Hospital Association last week.
MHA’s Workplace Violence at Massachusetts Healthcare Facilities: An Untenable Situation & A Call to Protect the Workforce shows that every 38 minutes in a Massachusetts healthcare facility, someone – most likely a clinician or employee – is either physically assaulted, endures verbal abuse, or is threatened. Following the report’s release, MHA Board of Trustees unanimously approved United Code of Conduct Principles to take a coordinated stand against violence in their facilities. The guidelines focus on the promotion of a safe environment, the nature of violations, potential consequences, and the ongoing maintenance of such policies. Anyone found violating the Code of Conduct may be asked to leave and future visits may be restricted. Organizations may alter the language and include additional items as appropriate for their individual facilities, but agree to uphold the principles as a united, baseline standard.
The AHA podcast that focuses on hospital codes of conduct features Christi Barney, R.N., vice president, Quality and Patient Safety, Emerson Health; Bonnie Michelman, executive director, Police, Security, and Outside Services at Massachusetts General Hospital and Mass General Brigham; and Patricia Noga, R.N., MHA’s vice president of Clinical Affairs.
In Memoriam: Carl Wathne
Carl Wathne, a former Chair of the MHA Board of Trustees and the founding director of the Massachusetts Community Hospital Association (now Massachusetts Council of Community Hospitals), passed away on April 9 at age 92. Wathne was Executive Director of Lahey Clinic in Boston and was instrumental in the formation of Lahey’s facility in Burlington. After Lahey, he served as president & CEO of Leominster Hospital.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association 