Federal Flexibilities, Drug Dispute, Vax Vote

INSIDE THE ISSUE
> Hospital at Home Advances
> Telehealth Uncertainty
> 340B Pilot Lawsuit
> Pediatric Vaccinations
> Women’s Leadership
MONDAY REPORT
Hospital at Home Waiver Sees Daylight…
The hospital community received a glimmer of good news from D.C. last Monday when the U.S. House voted unanimously to extend the Medicare Acute Hospital Care at Home waiver for another five years.
CMS established the hospital at home flexibility at the height of the COVID pandemic, easing Medicare restrictions so providers could bring acute-level inpatient care directly into patients’ homes. That waiver – and its subsequent extensions over the years – provided the foundation hospitals needed to launch and scale their programs, improving the patient experience and easing emergency department capacity in the process.
Hospitals were forced to pause their programs for several weeks as the waiver lapsed during the government shutdown. Congress voted within its Continuing Resolution to extend hospital at home until January 30, 2026 – which allowed providers to resume operations but did little to assure them that their programs would continue to enjoy federal support and predictability in the long-run.
Last week’s House vote, pending Senate approval and the president’s signature, would effectively ensure that much-needed sense of continuity for hospital at home programs through 2030. The bill would also direct the Secretary of Health and Human Services to conduct a study on what services hospitals are providing through the program, what patient populations are included, and how patient outcomes compare to inpatient services for the same conditions, and publish the results by the end of September 2028.
In Massachusetts, hospital at home services accounted for more than 4,500 discharges in 2024 alone. They were the subject of a Health Policy Commission research brief in October and a panel at the HPC’s Cost Trends Hearing last month.
“The number one thing we’ve asked for in terms of unlocking barriers to support our community and from a growth perspective…is obviously the federal waiver extension,” Constantinos Michaelidis, M.D., Medical Director of UMass Memorial Health’s Hospital at Home Program, told commissioners at the time. UMass Memorial’s program has cared for almost 4,000 patients since its launch and credits the model for decreasing readmissions among participants by 5 to 15% and reducing patients’ need for skilled nursing facilities by 80 to 90%.
Also last week, researchers at Mass General Brigham and Ariadne Labs released a study documenting hospital at home’s success for adults living in rural areas. Among a controlled trial of 161 participants in rural Illinois, Kentucky, and Canada, patients who received acute care services at home experienced higher satisfaction, greater physical activity, and lower costs than “brick-and-mortar” hospital participants.
…While Telehealth Still Hangs in the Balance
When the federal shutdown ended, another critical innovation that providers and patients have come to rely on was extended until January 30: Medicare telehealth flexibilities. But unlike hospital at home, the path forward for those telehealth policies is still unclear.
Federal lawmakers instituted a series of allowances during the pandemic that dramatically improved Medicare beneficiaries’ access to telemedicine. Those flexibilities have enabled patients to tap into virtual care regardless of their location (they previously had to be located in a medical setting and in a rural area). The policies have also allowed for wider use of audio-only services and expanded the types of providers who can deliver telehealth.
Without federal action by January 30, the dreaded “Medicare telehealth cliff” will emerge once again and the bipartisan-backed flexibilities will go away.
“We strongly urge Congress to immediately act on a long-term telehealth fix in its next legislative package to ensure stability and provide clarity for patients, providers, and the health care system as a whole,” a coalition of more than 450 healthcare organizations across the country, including the MHA-led tMED Coalition, wrote to congressional leaders last month.
While the pandemic has passed, the benefits of these flexibilities have become ingrained as a regular part of the patient experience and the everyday operations of providers. In addition to the obvious convenience factor, they have served as a bridge for people in rural and low-income environments – along with those with mobility and transportation challenges – to connect with advanced specialists and behavioral health professionals without the need for a previous in-person appointment.
A new research brief from the Brown University School of Public Health shows just how mainstream virtual care has become. 15% of Medicare fee-for-service beneficiaries in the country received at least one telehealth service in the first half of 2025. Massachusetts has emerged as a power user, with 23% of local Medicare patients utilizing telehealth within that time (second among all states). That usage dipped dramatically during the first two weeks of the recent shutdown.
Massachusetts’ recent application for the Rural Health Transformation Fund would support the expansion of both telehealth services and hospital at home programs for rural populations and providers, pending CMS approval.
Hospitals Sue HHS over Drug Pricing Pilot
When the federal government announced a new rebate-based pilot program for the 340B Drug Pricing Program in July, the concept was met with immediate resistance from hospitals, who viewed it as a slippery slope to more widespread erosion of the program. Now, several hospitals and hospital associations are formally seeking to block the pilot from getting off the ground ahead of its January 1 start date.
The American Hospital Association, the Maine Hospital Association, and four safety-net systems filed suit in a federal court last Monday, citing the rebate model as “unlawful, unnecessary, unexplained, and substantively unreasonable.”
340B was created in 1992 as a heavily regulated, bipartisan program requiring pharmaceutical manufacturers to sell outpatient drugs at discounted prices to healthcare organizations that care for uninsured and low-income patients. In the time since, it has become recognized as an essential component of the safety net system; hospitals and community health centers use the savings to provide low-cost prescription drugs to patients and to reinvest in their communities.
The rebate model would fundamentally shift how the financial underpinnings of the program work – starting with 10 drugs that were selected for the first round of Medicare drug price negotiations. It requires participating hospitals to pay manufacturers the full market cost for those 10 medications and then chase down reimbursement from the companies only once the drugs have been administered. 340B has been under increasing attack from well-funded pharmaceutical interests in recent years.
The Health Resources and Services Administration (HRSA) received more than 1,100 comments from concerned healthcare interests following its surprise announcement of the rebate pilot over the summer. Provider groups highlighted the enormous costs and administrative burdens they expect to endure as a part of the program – with no expected benefit to patient care or taxpayer dollars (340B savings are drawn solely from pharmaceutical profits).
“HRSA announced this mandatory Rebate Program with manifest disregard for the tremendous costs it will impose upon the most vulnerable covered entities—costs that HRSA recognizes in internal government documents will total hundreds of millions of dollars per year,” reads the lawsuit filed suit in the U.S. District Court for the District of Maine. “Astonishingly, when explaining its new Rebate Program, HRSA has not even acknowledged its own longstanding concerns about the massive costs of forcing a rebate model on safety-net providers…HRSA has given no public explanation of what it believes the costs are, what the benefits of the Rebate Program are, or why it is necessary to place those costs on the intended beneficiaries of the 340B Program— safety net healthcare providers that serve America’s most vulnerable patients.”
AHA and its co-plaintiffs argue that the model requires a more robust notice-and-respond period and allege that HRSA did not provide “reasoned responses” to providers’ concerns, as it is legally required to. They are asking the court to place a temporary restraining order on the program.
Mass. Stands Up to Slimmed-Down Vax Guidelines
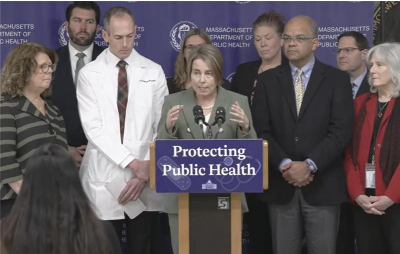
Flanked by local public health officials and medical experts, Governor Maura Healey last week – once again – issued a message that the state will rebuff new federal guidance and instead promote well-established vaccination practices for residents.
The Wednesday press conference was held just days before the CDC’s vaccine advisory committee was expected to recommend significant changes to the pediatric vaccine schedule – specifically around Hepatitis B. Sure enough, the Advisory Committee on Immunization Practices (ACIP) voted on Friday to recommend that newborns only receive a Hep B vaccine immediately if their mother is positive for the virus. Otherwise, parents should consult with their provider to determine “when or if” their child will be inoculated. CDC Acting Director Jim O’Neill must sign off on the recommendation.
Since 1992, the CDC has recommended administration of the Hepatitis B vaccine for all babies within 24 hours of their birth. Pediatric infection rates have dropped by 99% in that time, according to Department of Public Health (DPH) Commissioner Robbie Goldstein, M.D., who also spoke at the event.
“That is way more than a success story,” said Goldstein. “That is a home run. It’s one of the greatest public health interventions of our time. And it’s a shining example of what happens when science guides policy. And when prevention is embraced early, equitably, and universally.”
Massachusetts has responded to a cascade of changing public health guidance from the federal government in recent months. DPH issued its own vaccine recommendations and resources and helped launch the Northeast Public Health Collaborative to disseminate evidence-based public health policies.
“In Massachusetts…[we] will listen to science, we will be guided by our experts, and we will do all we can to protect public health for Bay Staters,” Healey stated, while assuring residents that “we’re going to make sure that [the Hep B] vaccine remains available here in Massachusetts.”

Women Leaders in Healthcare
MHA welcomed 500 attendees to its Annual Women Leaders in Healthcare Conference last Friday. Among the many highlights were an opening address from Lieutenant Governor Kim Driscoll, a panel of local women legislators, and a “fireside chat” between MHA Trustee and former Board Chair Christine Schuster, R.N. and the association’s incoming Board Chair, Anne Klibanksi, M.D.
“[Massachusetts] can figure out how we can continue delivering in an environment that is sometimes hostile to what we’re doing — and do it in a way that outperforms other places. And, dare I say, we are going to have to.”
– Lieutenant Governor Kim Driscoll
“We have an amazing membership of hospitals. And they’re different. Some are really big, some are small. Some are systems, some are individual hospitals. Some are financially healthier than others, although no one’s throwing a party. It’s thinking about those things collectively that we can come together around. Because there really is power in numbers. There is power in the group.”
– Anne Klibanski, M.D., President and CEO of Mass General Brigham, on her upcoming role as MHA Board Chair


 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association