Graduate Nurses, the NLC, and R.N. Needs Statewide

INSIDE THE ISSUE
> Graduate Nurses
> Nurse Licensure Compact
> FOCUS ON WORKFORCE: Lahey Hospital & Medical Center
> Change Healthcare
> February Transfer Delays
> Workforce Needs by State Region
> Transitions
MONDAY REPORT
Graduate Nurse Flexibility Included in Key Legislation
The Massachusetts House and Senate have both included in their respective supplemental appropriations bills (H.4466 and S.2708) language that extends the authorization for graduate nurses and nursing students in their last semester to practice at the bedside under appropriate supervision.
That authorization was created and extended during the pandemic to give hospitals the needed caregivers to deal with the influx of patients that crowded hospitals. Currently, with facilities at full capacity across the state, the workforce flexibility is needed more than ever. But without agreement between the two chambers on the spending bill, and a signature from the governor, the flexibility will end on March 31.
Both the House and Senate versions of their bills extend, at a minimum, the ability of the graduate nurses and nursing students to practice for one year until March 31, 2025.
Graduate nurses still must take the National Council for Licensure Exam-RN (NCLEX-RN), and they still must be licensed through the Board of Registration in Nursing. But allowing them to practice in the months before they are formally certified not only helps the new nurses get real-life experience, but helps the healthcare system, and the patients it serves, that is beset by record workforce vacancies.
Several overall differences in the competing proposals will need to be worked out before a final proposal is sent to the governor’s desk. MHA will be advocating for a quick resolution to ensure the graduate nurse flexibility remains in place without interruption.
Nurse Licensure Compact Still Needed; Opposition Argument Disproven
As demonstrated by the legislature’s recent action on supplemental spending bills (see related story above), graduate nurses are a critical part of the current healthcare workforce. A report last week from the Healey Administration (see related story below) showed that every region of the state identified the shortage of healthcare workers – especially nurses – as a key concern. Now, the region’s largest newspaper, the Boston Globe, has weighed in for the second time calling on the legislature to help easily resolve the commonwealth’s nursing shortage by passing the Nurse Licensure Compact (NLC).
The compact allows qualified nurses to have one license in their state of residency and to practice in other NLC states. Nurses participating in the compact are required to go through strict criminal history reviews and they have to meet all the licensing requirements of the states in which they want to practice. Forty-one states are currently part of the NLC, including three in New England.
Last Wednesday, the Globe reprised its call from July 2022, urging the legislature to approve Massachusetts’ inclusion into the NLC. In an editorial entitled “Massachusetts needs more nurses and should ease path for out-of-state workers,” the Globe wrote: “[J]oining the compact could help Massachusetts adapt to unforeseen changes in nursing needs that require temporary staffing, like a natural disaster or pandemic or seasonal fluctuations, like an influx of summer visitors to Cape Cod. It would make it easier for nurses who live in neighboring states to work in Massachusetts. (Today, a nurse licensed in another state needs to apply for a reciprocal license to work in Massachusetts.) With the rise of telehealth, joining the compact would make it easier for Massachusetts patients to receive telehealth care from out-of-state nurses and for Massachusetts nurses who care for out-of-state patients to provide follow-up care. This could be important if a New Hampshire resident has surgery in Massachusetts or a Texas resident has an abortion here. It could allow more nurse educators to teach remotely, amid a shortage of nursing faculty.”
The Health Policy Commission has endorsed the NLC as has the post-acute care community, the Organization of Nurse Leaders, and numerous other healthcare and patient safety voices. The main argument against the NLC – namely, that there already are enough nurses in Massachusetts – has been disproven. All sectors of the healthcare system – from school nurses to M.D. offices to walk-in clinics to positions at well-paying hospitals – are in search of nurses.
FOCUS ON WORKFORCE
Fostering a Culture of Health & Wellbeing Benefits from a Dedicated Team

Kristen Bedrick, R.N., the director of health and wellness at Lahey Hospital & Medical Center (LHMC), is keenly aware healthcare workers approach stress and wellness differently. Their actions and reactions, she says, can vary by gender, age, professional experience, and more. Even an individual’s own outlook on stress and wellness, she notes, can change from day to day, depending on what the worker is experiencing at any given time.
But a certainty, Bedrick says, is if hospitals and health systems want to address the wellbeing of their workforce completely and effectively, they must create a dedicated wellness team. Layering wellness duties on to other roles is not adequate, she says.
“The benefit of having a dedicated wellness team is that it keeps the issue near the top of the priority list – and hospitals have a lot of priorities,” Bedrick says. “It serves as a reminder that we should always be viewing operations and experiences through the lens of wellbeing and to consider how the colleague will be affected by the initiatives and priorities we’re focused on as an organization.”
LHMC’s Health & Wellness Department goes beyond simply strengthening workers’ personal resilience, Bedrick says. It also addresses efficiencies of practice throughout the organization, such as reviewing staffing levels and opportunities to streamline operations so each colleague can focus on their primary roles. While Bedrick says it’s important to take care of frontline staff – “To give the best patient care, the caregivers need to be well,” she says – the hospital’s initiatives are intended for staff at every level of the organization, including contractors and volunteers. Read the full story here.
Learn about other workforce initiatives throughout the state by visiting MHA’s Workforce Toolkit. Do you have a workforce program that you would like featured in the toolkit? Contact MHA’s Kim Stevenson at kstevenson@mhalink.org.
Local Coordinated Effort Addresses Change Healthcare Cyberattack
The MassCollaborative launched a series of services last week to assist providers affected by the Change Healthcare cyberattack that is still ongoing and causing significant disruption to providers across the state. Hospitals are still continuing to lose millions of dollars in reimbursement each day that must be recouped.
A toll-free helpline and a webpage were created to assist providers with setting up alternate electronic data interchange services to file claims. Checklists and a frequently asked questions page were also sent to members of the MassCollaborative, which is made up of MHA, Massachusetts Medical Society, Massachusetts Association of Health Plans, Blue Cross Blue Shield of Massachusetts, and the Massachusetts Health Data Consortium.
Even after UnitedHealth Group, the parent company of Change Healthcare, succeeds in making nominal re-connections, health plans and providers will require additional time to test new connections and ensure their security.
Also last week, the American Hospital Association and the Federation of American Hospitals urged the Department of Health and Human Services’ Office of Civil Rights (OCR) to clarify that Change and United – not hospitals and other downstream victims of the cyberattack – should be responsible for issuing breach notifications to patients.
“OCR must preemptively relieve hospitals and other providers of any potential breach notification burdens, which would cause significant patient confusion and undoubtedly be costly and resource-intensive,” AHA and FAH wrote.
Throughput Challenges by Region, Care Type, Insurance, and More
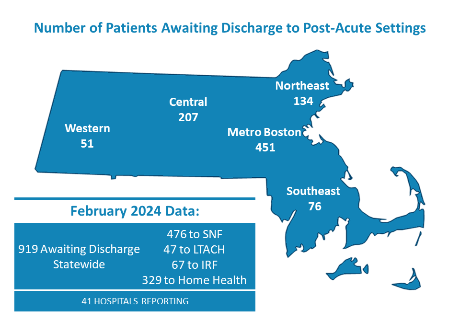
MHA’s February 2024 Throughput Survey Report – a point-in-time questionnaire to hospital case managers asking how many patients in their facilities are awaiting discharge to a post-acute facility or services – showed 919 patients were stuck in just 41 of the hospitals that responded to the MHA survey. When patients cannot transition out of an acute care hospital bed, other patients boarding in hospital EDs or in medical/surgical units awaiting that occupied bed have nowhere to go.
The survey showed that 43% of patients awaiting to be discharged to a skilled nursing facility were waiting for 30 days or more.
The report details the types of beds needed (short-term, Alzheimer’s care, geriatric-psych, etc.) to fulfill the demand, the types of insurance coverage for patients awaiting discharge, and discharge delays by region of the state, among many other metrics.
Workforce Plan Notes Healthcare Shortages Across the State
The Healey Administration last week released a statewide workforce agenda, entitled Meeting the Moment to Attract, Retain, and Develop a Future Workforce.
One part of the report focuses on the seven regional Workforce Skills Cabinet Teams that prioritized industries and occupations most needed in their parts of the state. Nearly all sectors placed “healthcare and social assistance” workers at the top of their priority needs.
About the health sector, the report notes: “Massachusetts has been experiencing disruption in healthcare and human service delivery at unprecedented levels since the COVID-19 pandemic. Workforce issues that existed before the pandemic have only become exacerbated, impacting talent attraction and retention plus patient care across the commonwealth. Healthcare is the largest employment sector in Massachusetts, employing 477,704 workers; the human services sector employs approximately 160,000 workers.” MHA surveys have shown that there are approximately 19,000 vacant full-time positions in Massachusetts hospitals and health systems alone.
Joanne Pokaski, assistant vice president of workforce planning and development for Beth Israel Lahey Health, chairs the MassHire Workforce Board that along with the Executive Office of Labor and Workforce Development was instrumental in creating the report. The outline of the administration’s workforce development plan is part of the Workforce Innovation Opportunity Act State Plan that Massachusetts must submit every four years to the federal Departments of Labor and Education.
Transitions
Allen Smith, M.D., the president & CEO of South Shore Health, is the newest member of the MHA Board of Trustees, which met last Thursday. Smith has led South Shore since November 2020. Before that he was president of the 1,800-member Brigham and Women’s Physicians Organization.
***
Michael Gustafson, M.D., has been named CEO of the Schwartz Center for Compassionate Care. Gustafson most recently was president of UMass Memorial Medical Center and before that he was president/COO of Brigham and Women’s Faulkner Hospital. During his hospital leadership roles, Gustafson served on the MHA Board of Trustees, chairing the association’s Clinical Issues Advisory Council (CIAC).
***
Massachusetts Insurance Commissioner Gary Anderson will become CEO of the National Association of Insurance Commissioners, effective May 1. Former Governor Charlie Baker appointed Anderson to lead the Division of Insurance in October 2017.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association