Healey: 250,000 May Lose Coverage

INSIDE THE ISSUE
> Leaders Speak Out on Medicaid Cuts
> Sen. Warren on House Bill
> MAVRIC Goes Live
> Improving the EMS System
> Insurer Merged Market Increases
> CMS Enforcement
> New COVID-19 Vax Recommendations
MONDAY REPORT
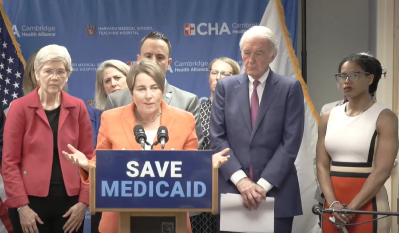
Healey: 250,000 Would Lose Coverage Under House Bill
Political and health leaders gathered at Cambridge Health Alliance’s Revere Care Center last week to show how the Medicaid cuts contained in the recently passed U.S. House bill would lead to more than 250,000 people in Massachusetts losing health coverage, as well as destabilize hospital, community health center, and nursing home finances.
“This is not, as [Republicans in Congress] would describe it, a scalpel,” Governor Maura Healey said. “We’ve heard that term before – ‘a scalpel to a problem.’ It really is just a blunt force axe, and it’s going to fall on a lot of people here in Massachusetts and a lot of people around this country. People will get hurt and people will die and it will raise costs for everyone else. If this cut goes through, a quarter of a million people in Massachusetts will lose their healthcare coverage.”
The governor added that the Medicaid cuts contained in the House bill will cut $1.75 billion from the Massachusetts healthcare system.
Governor Healey was joined at the event by U.S. Senators Elizabeth Warren and Edward Markey, State Senator Lydia Edwards, and Revere Mayor Patrick Keefe, among many others all describing the immediate effects on Massachusetts healthcare if the House-passed bill does indeed become law.
“Instead of fighting for guaranteed healthcare for all, Republicans in Congress are trying to gut Medicaid and rip healthcare away from millions of children and seniors in Massachusetts, and across the country – all to pay for tax breaks for billionaires,” Senator Markey said. “But the fight to save Medicaid is far from over. We cannot agonize – we must organize to reject this big billionaire bonus and fight for a health care system that works for all Americans.”
The U.S. Senate is now crafting its own tax-and-spending bill that Senate leaders have indicated will be separate and distinct from what the house did. Those speaking at the Revere event last week said that it is imperative before the Senate acts to clearly detail what’s at stake with proposed Medicaid cuts.
Sen Warren Details How the U.S. House Bill Would Affect Care, Economy
U.S. Senator Elizabeth Warren, at the “Save Medicaid” event last week in Revere, delivered the following answer to a question from the media.
Q: “Senator you talked about the wealth transfer aspect of this bill. Beyond the people who are directly, potentially going to lose their insurance, could you talk about just, societally, beyond those who use Medicaid, how this affects wealth transfer?”
A: “First is that the hospitals and community health centers that currently provide services get full reimbursement from the Medicare and Medicaid programs. When they lose that reimbursement that means that the very slim margin that is the difference between operating in the black and operating in the red is gone. And these hospitals – some of which are holding on right now by their fingernails – end up closing. When they close, they don’t just close for Medicaid patients. They close for everybody. So anybody who’s feeling chest pains and needs emergency medical care right now is just out of luck. Anyone whose kid falls at the playground and needs what looks like 126 stitches is just out of luck. Anyone who’s looking to deliver a baby is just out of luck. So that’s how it starts to echo through the system.
“The other way it echoes through the system is that providing alternative ways to get access to healthcare is part of how people are able to start their own businesses. You know, not everybody is going to work for a giant corporation, and if you’re not working for a giant corporation that can actually help you with healthcare then you’ve got to rely on these other systems that work through the government. So [for] everybody who wants to start a little business, one of the first questions they have to ask is ‘What’s my idea for the business? How am I going to get financing? And how am I going to pay for my healthcare during the time that I’m trying to get this business up and running?’ You take away these supports and you take away much of what entrepreneurs rely on to be able to get those businesses up and running.
“Third way that it hurts is look at all of the people right now who are working … many of them are working two and three jobs but it’s not enough [for them to receive] full coverage healthcare. So they’ve got to rely on programs like Medicaid in order to be able to be able to stay in those jobs and to take care of themselves and their kids when somebody gets sick. You lose that and now you’ve got more people who are back in the hospitals for uncompensated care and, more to the point, they’re not getting the healthcare they need when they need it. It is cheaper to take care of the child when the tooth first hurts rather than after an infection has set in. And that’s true all the way through the healthcare system.
“And then I will mention the last one – although there are more – and that is for people with significant disabilities who need that home health aide.” Senator Warren referenced Dennis Heaphy, a health justice advocate at the Disability Policy Consortium, who spoke earlier of the importance of MassHealth in allowing him to receive care at home for his complex medical needs. “The difference between Dennis getting some help so that he can stay in his own home in his own apartment and having Dennis have to go to a facility that will provide round-the-clock care for him is a difference not just of quality of life for Dennis, it’s also a straight dollars-and-cents difference. It costs more money for Dennis to have a tougher, more restricted life in a nursing home than it does for him to be in his own home. We make that happen through these federal supports that we keep in place. If Dennis’s home health aides are gone, then Dennis is off to a nursing home. And we have traded something that is barely working for something that is just not going to work. And that echoes through our whole commonwealth. And that’s only just some of it.”
MAVRIC Goes Live Today at 9:30 A.M.
The Massachusetts Vital Records Information Collaborative (MAVRIC) system will go live today, Monday, June 2, at 9:30 a.m. MAVRIC is the new electronic filing system that has been in the works for the better part of a year. It replaces the more cumbersome and limited Vitals Information Partnership (VIP) system.
Implementing the MAVRIC system was a complex endeavor in that it involved the healthcare community, as well as town clerks, funeral home operators, and others involved in the death registration process. Extensive online training was required for the new system.
As of today, all new death records must be started in MAVRIC. Any records in progress in the old VIP system must be completed in VIP, so users are encouraged to not disable VIP in their systems.
VIP will remain active through Monday, June 30 and will be deactivated at 5 p.m. on that day.
Legislative Focus:
Pending Bills Can Help Repair the EMS System
Across the commonwealth, the shortage and underfunding of Emergency Medical Services (EMS) has resulted in a steady and serious disruption of the healthcare system.
EMS is an essential component of the entire continuum of care. In addition to their “first-on-the-scene” role in responding to emergencies, EMS personnel are involved in mobile integrated health, and in providing mental health services often in partnership with behavioral health professionals and sometimes law enforcement.
But the EMS system is facing the same issues currently affecting the hospital and health system sector, including staffing shortages, reimbursement issues, and rising operational costs.
Many EMS providers are struggling to maintain 24/7 service, particularly in rural and under-resourced areas. As a result, hospitals are experiencing discharge delays, patients face longer wait times for non-emergency transport, and behavioral health patients often remain in emergency departments longer than necessary due to a lack of appropriate transport options. These system-wide delays contribute to overcrowded emergency rooms, postponed care, and increased stress for patients, families, and healthcare workers.
In response, MHA has put forth several bills in the current legislative session to stabilize and modernize EMS in Massachusetts.
H.1198 / S.746 : An Act to Improve Patient Access to Non-Emergency Medical Transportation, filed by Rep. Dan Hunt (D-Boston) and Sen. Paul Feeney (D-Foxborough), would address growing EMS challenges by ensuring insurance prior authorization for patient transportation is valid for three business days. This allows any transport delays to be considered, while ensuring that EMS providers are adequately reimbursed by MassHealth for non-emergency medical transportation for behavioral health, dialysis, and post-acute care transportation.
H.2491 / S.1513 : An Act Establishing a Task Force to Study the Sustainability of Emergency Medical Services, filed by Rep. John Mahoney (D-Worcester) and Sen. Bill Driscoll (D-Milton), would establish an EMS task force to issue a report and recommendations on ways to ensure that the commonwealth’s EMS capabilities are met.
H.2234 / S.1397 : An Act Establishing Alternative Models for Behavioral Health Transport, filed by Rep. Adam Scanlon (D-North Attleboro) and Sen. Feeney, would require the Executive Office of Health and Human Services to establish a pilot program to evaluate alternative models of transport for behavioral health patients and would require that MassHealth reimburse for these services. Traditional EMS models, primarily designed for acute medical emergencies, are not designed to address the nuances of behavioral health diagnoses or the statewide behavioral health system, leading to long response times, overcrowded facilities, and a lack of specialized care during transport. Alternative transports improve outcomes, reduce strain on EMS systems, and offer a more humane, effective response to behavioral health transport. The importance of establishing such a system was highlighted in a recent Boston Globe editorial .
Health Insurer Proposed Increases for Merged Market Average 13.4%
State law and regulations require that every health insurer offering coverage in the “merged market” (that is, individuals and small businesses up to 50 eligible employees) must submit their proposed premium rates to the Division of Insurance (DOI) by May of each year. As of December 2024, there were 711,563 consumers enrolled in merged market plans.
For 2026, the proposed average rate increases for the eight insurers offering products in the Massachusetts merged market is 13.4%; the requested increases range from 9.9% to 16.2%. By comparison, the approved average rate changes were 4.8% in 2024 and 7.8% in 2025.
In their filings , most of the insurers noted that rising pharmaceutical costs, particularly for GLP-1 drugs, contributed greatly to the proposed increases. The insurers noted that providers attributed cost increases to labor shortages, the effects of inflation, and the need to compensate for the lower Medicaid reimbursement rates on the insurers’ Medicaid line of business.
DOI is now reviewing the filings and may disapprove the proposed increases if it finds that rates are not reasonable in relation to health plan benefits, or if they are excessive or inadequate, or if they use rating factors that are discriminatory or not actuarially sound. In addition, as part of the 2026 filing, the Division will expect health insurers to include an explanation of how their filings address “affordability for consumers and purchasers of health insurance products.” DOI is holding a public information session on the filings on June 17 at 9 a.m.
CMS to States: Review the Care Provided to Undocumented People
The Centers for Medicare and Medicaid Services (CMS) sent a letter to all states last week saying that it would not tolerate the use of federal funds “to pay for or subsidize healthcare for individuals with an unsatisfactory immigration status.” The letter from Drew Snyder, CMS deputy administrator and director, said, “Federal Medicaid funding is generally only available for limited Medicaid coverage necessary for treatment of an emergency medical condition, including emergency labor and delivery, and not related to an organ transplant procedure, for individuals who meet all Medicaid eligibility requirements except satisfactory immigration status.”
The letter encourages states to “review their policies, internal controls, public assistance cost allocation plans, and IT systems to ensure that the state is claiming medical assistance and administrative expenditures in accordance with federal law.”
New Vaccine Recommendations Sow Some Confusion
U.S. Health & Human Services Secretary Robert Kennedy announced, through a video on X last Tuesday, that “as of today, the COVID-19 vaccine for healthy children and healthy pregnant women has been removed from the CDC recommended immunization schedule.”
As of Friday, however, the CDC website detailing vaccine recommendations for pregnant women stated “COVID-19 vaccination remains the best protection against COVID-19-related hospitalization and death for you and your baby. CDC recommendations align with those from professional medical organizations, including the American College of Obstetricians and Gynecologists, Society for Maternal Fetal Medicine, and American Society for Reproductive Medicine.”
On Friday, the CDC did change its childhood recommendations page. However, it did not remove the COVID-19 vaccine from the schedule entirely; rather the page now states that for healthy children aged six months to age 18, vaccines are available through “shared clinical decision making.”
The CDC guidance states: “Shared clinical decision making vaccinations are individually based and informed by a decision process between the healthcare provider and the patient or parent/guardian. Where the parent presents with a desire for their child to be vaccinated, children 6 months and older may receive COVID-19 vaccination, informed by the clinical judgment of a healthcare provider and personal preference and circumstances.”
Some advocates have questioned whether vaccines received through shared decision making would be covered by insurance.
In his Tuesday announcement, Kennedy said there is a “lack of clinical data” to support the vaccines in healthy children and pregnant woman. He made the announcement flanked by National Institutes of Health Director Jay Bhattacharya, M.D., and U.S. Food and Drug Administration Commissioner Martin Makary, M.D. Not included was a representative from The Advisory Committee on Immunization Practices (ACIP), which is tasked with developing recommendations on how to use vaccines to control disease in the United States. ACIP recommendations become official CDC policy once adopted by CDC’s director. The CDC currently does not have a director. The most recent ACIP guidance, issued in December 2024, states that all persons over six months old should receive the 2024–2025 COVID-19 vaccination. ACIP is next scheduled to meet June 25-27. ACIP members typically serve four-year terms, but they are appointed by the Secretary of Health and Human Services, who can appoint and dismiss members at will.


 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association