INSIDE THE ISSUE
> Hospitals Help Build Jobs, Economy
> Telehealth Extension
> Cost Trends Hearing
> Respiratory Illness
> Quote of Note
> Schwartz Center Dinner
> Transition: Barbra Rabson
MONDAY REPORT
Massachusetts Hospitals Add 10,000 Jobs and Reduce Workforce Shortages
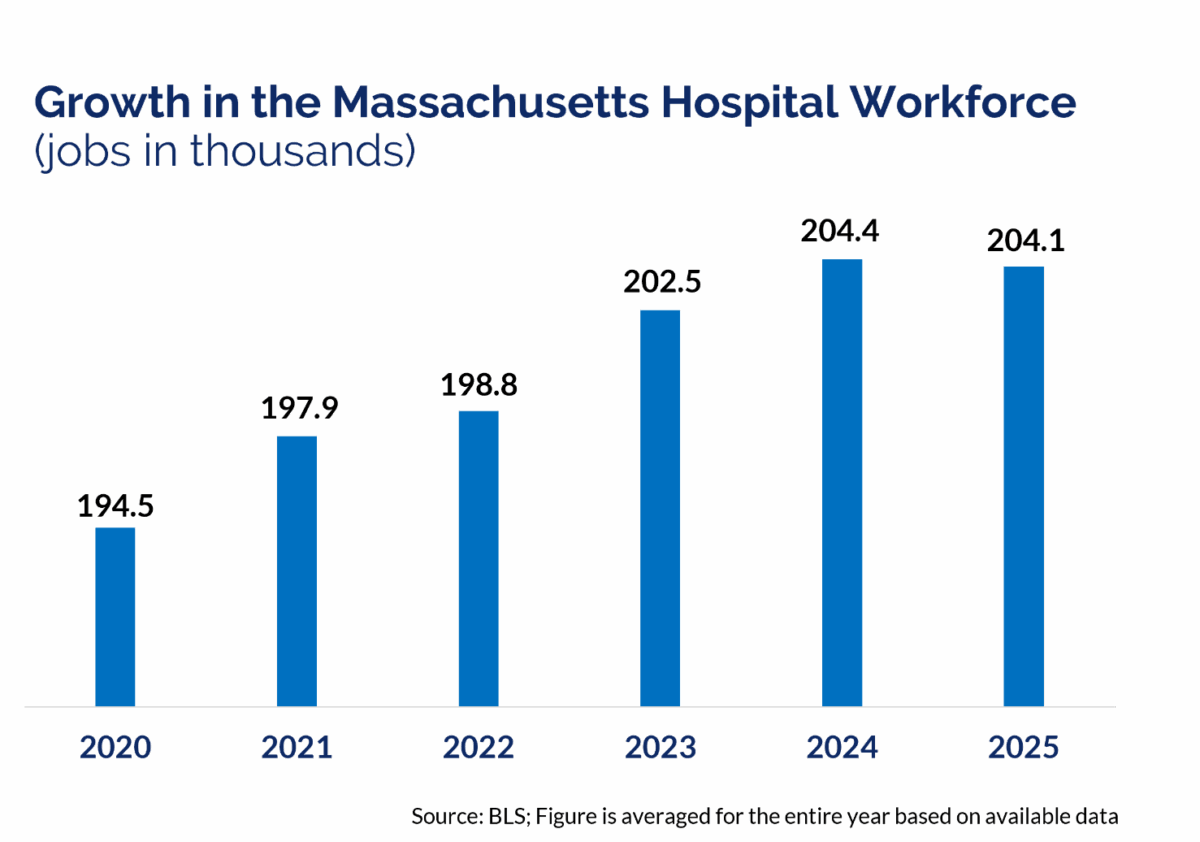
Massachusetts hospitals have made major progress in building and strengthening the state’s healthcare workforce in recent years, according to an MHA report released today.
On the Mend: Progress and Pressure Points for Massachusetts’ Healthcare Workforce shows that Massachusetts hospitals have added 10,000 jobs since 2020, helping cement the sector’s status as a leading economic engine for the state. Following MHA’s 2022 workforce report identifying 19,000 vacancies in key hospital positions across the commonwealth, On the Mend reveals that focused recruitment, hiring, and retention efforts have reduced that number to 13,600 open positions – a 28% decline.
“This is a remarkable success story – not just for healthcare, but for all of Massachusetts,” said Valerie Fleishman, executive vice president and chief innovation officer at the Massachusetts Health & Hospital Association. “Even through enormous operational challenges, our hospitals and health systems have devoted a record amount of resources to workforce in recent years. These investments have made a clear difference, and they deserve to be celebrated as a sign of our commonwealth’s success. Every one of these 10,000 new jobs improves care access for a patient, supports a local community, and provides a true livelihood for a friend or neighbor.”
Hospitals are a major source of stable, well-paying jobs and are expanding their hiring to meet the ever-rising need for care. This growth has occurred within a highly volatile financial landscape – both for the healthcare community and other sectors.
Nursing roles saw some of the sharpest improvements from 2022 to 2024. Five of the 10 largest vacancy reductions occurred in nursing positions, and the statewide nursing vacancy rate has dropped from 15% to 10%. Hospitals also report a steep decline in the use of high-cost “travel nurses” from 2023 to 2024, though temporary labor remains higher than pre-pandemic levels.
The report highlights the success of coordinated statewide actions and collaboration among hospitals, their partners, and state government. Hospitals and health systems have built new academic partnerships and training programs while expanding career ladders, increasing salaries and benefits, and expanding wellbeing programs for existing workers. State leaders have passed funding to develop the behavioral health workforce, launched free community college opportunities, and scaled up local job training programs, among other actions.
“It’s no coincidence that the voices of nurses and caregivers have been at the heart of our recent strides,” said Nancy Gaden, DNP, R.N., FAAN, senior vice president & chief nursing officer at Boston Medical Center and co-chair of MHA’s Workforce Leadership Task Force. “Through MHA’s Task Force, we have assembled an academy, removed stigmatizing questions from the credentialing process, and mounted a messaging campaign – all within the course of just a few years. We will continue to amplify the perspective of our frontline providers as we build a more resilient, supportive workplace of the future.”
Healthcare providers, however, continue to navigate persistent shortages in some patient-facing roles. The report documents the high vacancy rates still being seen among technicians, community health workers, certain behavioral health professionals, and advanced practice providers – positions that are critical to patient care.
Maintaining the momentum Massachusetts has built over the past several years will be essential to addressing remaining workforce gaps, particularly for roles that are well above the median vacancy rate of 14.2%. On the Mend outlines policy reforms, targeted statewide strategies, and trainings opportunities that Massachusetts can embrace with these high-need positions in mind.
The data presented in the report is derived from a survey sent to hospitals in early 2025 requesting information on 56 positions. It is worth noting that, concurrently with the uptick in hiring, certain, largely non-clinical roles have faced layoffs due to the financial pressures besetting the entire healthcare ecosystem in the commonwealth. Based on MHA’s data, the reduction in vacancy rates for these key surveyed positions (the vast majority of which are clinical or patient-facing) was primarily the result of new hires in those areas.
450 Sign Letter Urging Long-Term Telehealth Extension
The government remains shut down and the U.S. House has been in recess since September, but that hasn’t stopped health interests from stressing the need to pass immediate telehealth relief as soon as the business of governing resumes.
Last week, 450 healthcare sent a letter to Republican and Democratic leaders of the House and Senate, urging them to pass a long-term extension of telehealth flexibilities in Medicare. Among those signing was tMED – The Massachusetts Telemedicine Coalition, consisting of 50 groups in Massachusetts convened by MHA, as well as Mass General Brigham and Massachusetts Health Data Consortium.
The letter notes that Congress has only been providing short-term extensions of the telehealth flexibilities when up against the deadline of their expiration, but that the recent shutdown has demonstrated the unsustainability of this practice. With the expiration of telehealth flexibilities triggered by the government shutdown, 30% of healthcare providers across the country are facing disruptions to their delivery of care to Medicare beneficiaries, the letter notes. As a result, the coalition asks that Congress ensure that providers and patients are provided with long-term and predictable access to telehealth services and that “practitioners that maintained patient access to critical services during this lapse” receive retroactive payments. Nearly 350 health groups sent a similar letter to Congressional leaders in August when Congress was discussing the continuing resolution (CR). The failure to pass that CR resulted in the shutdown.
Wednesday’s Cost Trends Hearing: A Focus on Prior Auths?

The Health Policy Commission holds its annual cost trends hearing this Wednesday, November 12.
The annual, full-day cost trends hearing combines research presentations with various panels all dedicated to figuring out how to maintain a vibrant, accessible, and equitable healthcare system while lowering the costs needed to sustain it.
The 2025 hearing is different from previous years in that in addition to required testimony from providers and payers, pre-filed testimony is now required from pharmaceutical manufacturers, pharmacy benefit managers, equity investors, real estate investment trusts, and management services organizations. Among those testifying will be Michael Lauf, president and CEO of Cape Cod Healthcare and MHA Board Chair on a panel entitled “State Strategies to Promote Affordability, Access, and Equity;” and Kevin Tabb, M.D., president and CEO of Beth Israel Lahey Health on a panel entitled “How CEOs are Maintaining a Focus on Affordability in a Time of Uncertainty.”
A theme running through all the panels and in the questions the HPC posed to those submitting written testimony is how recent federal actions will affect Massachusetts healthcare. Another persistent theme in this and previous cost-trends hearings is how “administrative complexity in the healthcare system can burden clinicians and patients and contribute to burnout, reduce timely and equitable access to care, and add unnecessary costs to the system.”
Pre-filed provider testimony includes the following statements from hospitals across the state:
- “Our clinicians, case managers, and social workers continue to face challenges on prior authorization and delays in authorization by payers. The rates of technical and unsupported denials are unacceptably high … This adds to patients unnecessarily boarding in hospitals and delayed care.”
- “Administrative complexity in the healthcare system frequently creates delays in care that burden all patients, but which can disproportionately affect cancer patients who often have complex and acute illnesses … Many health plans today are using prior authorization in ways that lead to delays in care, dictate suboptimal treatments, and create unnecessary stress for both patients and clinicians.”
- “Often, there is conflicting information … resulting in patient, provider, and facility disconnect around the authorization requirement. This work leaves an unsettling lag time where the patient has a healthcare need ordered by his/her provider, that is being delayed by an administrative task.”
- “Without question, the prior authorization process and onslaught of denials by insurers are the most challenging for us. Some progress has been made with prior authorizations, but more needs to be done. Insurers are also increasingly using AI to deny claims often resulting in lengthy and costly appeals processes.”
History Says Flu and COVID-19 Season About to Really Begin
So far, on the respiratory illness front, things are pretty good.
Emergency department visits and hospital admissions for respiratory illnesses – including the flu, RSV, and COVID-19 – are below previous years’ rates at this time. But historically, incidences of respiratory illnesses do not really begin to move upwards until later in November and into December, with the peaks usually occurring in January and February. Which means that right now is an especially important time to get vaccinated against respiratory ailments. The state’s respiratory illness dashboard tracks all the data.
DPH recommends that everyone six months of age and older receive a 2025-2026 COVID-19 vaccine, and that those at the highest risk – those 65 years and older, children six months to two years, and people of any age with underlying medical conditions – should definitely get vaccinated. DPH also recommends an annual flu vaccine for everyone six months of age and older, and that people over 50 should discuss with their doctor if they should get an RSV vaccine.
State licensure regulations for hospitals and other healthcare facilities requires them to ensure that all healthcare personnel receive flu and COVID-19 vaccines. And DPH expects that hospitals will provide vaccinations to any admitted patient who has not yet received them.
Here’s DPH’s vaccine information for the general public, and here is info for healthcare providers.
Quote of Note
With impending federal cuts and the need to adequately fund a host of programs, one of the state’s chief budget writers expressed his concerns last week.
“We certainly have concerns, based off of how volatile everything is with the federal government, and the reimbursement conversation that would be taking place around that, and then certainly with the [Medicaid] eligibility changes that we are certainly concerned about going into next year as a result of the federal bill that was passed earlier this summer … It’s part of a bigger discussion point that we’re having here, related to [the Supplemental Nutrition Assistance Program], related to potentially [the Low Income Home Energy Assistance Program]. None of this is in individual silos. We have to look at this as a bigger picture conversation about how we can afford these things and how we’re going to handle keeping our budget stable.”
– House Ways and Means Chair Aaron Michlewitz (D-Boston) as quoted in the State House News Service
November 18: 30th Annual Schwartz Center Dinner
The 30th Annual Kenneth B. Schwartz Compassionate Caregivers of the Year Award will be presented on Tuesday, November 18 at the Schwartz Center dinner at SoWa Power Station in Boston. The keynote speaker will be Stephen Trzeciak, M.D., co-author of Compassionomics: The Revolutionary Scientific Evidence that Caring Makes a Difference. The event runs from 5:30 to 9 p.m. Purchase tickets here.
Transition: Rabson to Leave MHQP
Barbra Rabson, who has led MHQP since April 1998, announced last week that she will step down from her role in the summer of 2026. MHQP was established in 1995 through the leadership of MHA Board Chair H. Richard Nesson, M.D., and a group of local healthcare leaders. Three years later, Rabson was named to lead the group and released the first-in-the-nation statewide survey of patient experiences in hospitals. Under her leadership, MHQP elevated the patient voice throughout the Massachusetts healthcare system and in recent years began to stratify data by race and ethnicity to identify the systemic issues driving disparities and to compare performance across organizations. “This is a challenging time for healthcare, and the independence and dedication to improving healthcare quality in Massachusetts that MHQP has demonstrated over its 30-year history is needed now more than ever,” Rabson stated in the notice announcing her decision. WittKieffer is leading the search for MHQP’s next president and CEO.


 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association 