Hospitals Rang In New Year with Dismal Finances

INSIDE THE ISSUE
> Omicron Affected Financials
> Masking
> Budget Debate Begins Today
> UMass’ Foster McGaw Recognition
> Postpartum Care
> June 2: CARe Forum
MONDAY REPORT
Omicron Hammered Hospital Financials at Start of 2022
During January and February of this year, the vast majority of Massachusetts acute care hospitals showed negative operating margins even with COVID-19 relief funds from the federal government.
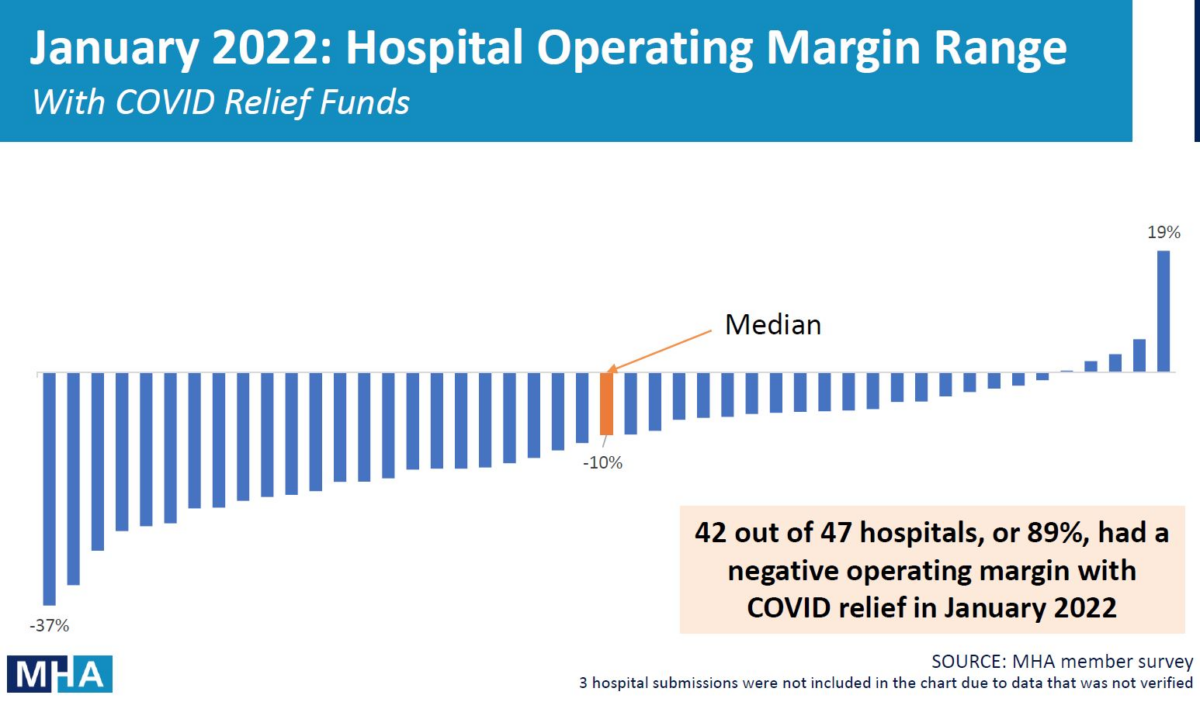
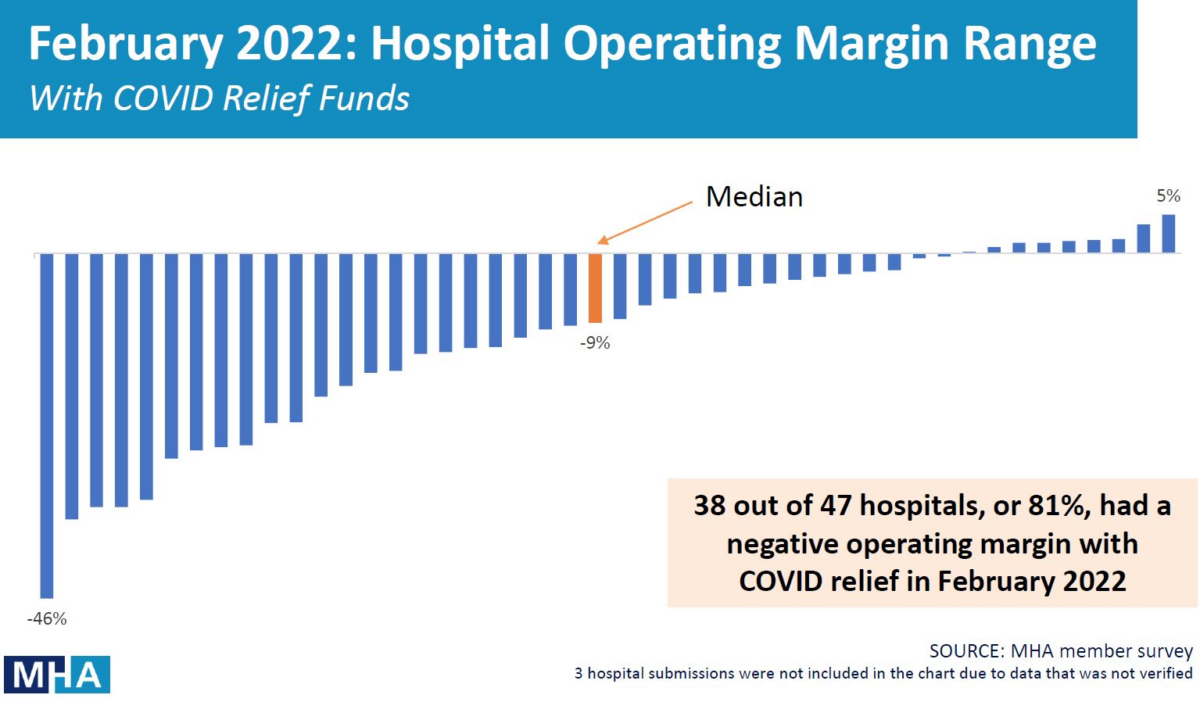
The hospital data shows that 42 of 47 (or 89%) of reporting hospitals in January, and 38 of 47 (81%) in February lost more money than they took in. The median operating margin in January and February 2022 was negative 10% and negative 9%, respectively.
All totaled, Massachusetts responding hospitals lost $262 million in January 2022 and $168 million in February 2022, or a massive $430 million total to begin the year.
Last Thursday, Governor Charlie Baker released a $3.5 billion economic development bill, which contains $2.3 billion in funding from the federal American Rescue Plan Act (ARPA). Baker’s bill dedicates $250 million for fiscally distressed hospitals.
MHA President and CEO Steve Walsh said hospitals were “tremendously grateful” for the relief proposal and noted that “the financial pressures brought on by the pandemic have not gone away, and they were quickly compounded by the Omicron wave earlier this year.” He added, “It is clear that these hospital losses are simply unsustainable as healthcare organizations strive to remain fully accessible to the millions who rely on their care.”
Throughout the pandemic, providers lost billions in revenue and experienced new expenses. Cost pressures included expenses related to emergency preparedness, personal protective equipment, capacity planning and implementation, supply chain disruptions and shortages, the curtailment of planned procedures, testing and vaccine administration, and challenging dynamics surrounding care delivery. The pandemic also intensified workforce challenges, which resulted in significant increases in hospital labor expenses, including exorbitant costs to travelling nurse and staffing agencies — costs that are continuing into 2022. Like the rest of the economy, the healthcare sector is now facing substantial inflationary cost pressures in all areas of operations that greatly exceed historic economic growth rates.
The state’s Center for Health Information & Analysis tracks hospital finances but the last report covered the October through December 2021 quarter; that report showed 19 out of 49 hospitals with negative operating margins and a statewide median margin of only 1.4%. Since then, Omicron has wreaked havoc on finances. The next CHIA report, however, will cover the period between October 2021 through March 2022, and its cumulative perspective will mask the unprecedented nature of the January and February 2022 losses, prompting the need for the MHA survey.
“Our elected leaders understand these pressures and have been there for hospitals and their caregivers every step of the way,” MHA’s Walsh said. “We appreciate the ongoing work of the state legislature to provide additional relief, and we will continue to rely on their support as we work to restore the long-term stability of the system.”
Hodgepodge of Masking Directives
The issue of masking against COVID-19 transmission is in flux. Last Monday, a federal judge in Florida struck down the federal government’s mask mandate for mass transit, saying the CDC had exceeded its authority in issuing the mandate and had not followed the proper administrative procedures in reaching its decision. On Wednesday, the U.S. Department of Justice stated it would appeal the judge’s ruling after the CDC said it still maintains that masking on public transport “remains necessary for the public health.” In the weeks before the court order, the CDC had extended the transit mask mandate through May 3.
While the issue plays out in the courts, many airlines and transit systems across the U.S. eliminated the masking mandate. The MBTA, for example, said last Tuesday, “beginning today, the mask mandate on MBTA vehicles and MBTA properties will be lifted for all MBTA customers.” Yet many passengers, aware of the persistent infection rates and leery of being in cramped subway cars and buses with others, naturally continued to wear masks.
The Boston Public Health Commission last week recommended that people should once again wear masks indoors. The BPHC wrote: “COVID-19 cases have increased by 65% in the past two weeks and community positivity has climbed to 6.9% after being as low as 2.2% in early March. The amount of COVID-19 particles in local wastewater samples has increased by 109% over a 14-day period, suggesting that cases could continue to rise in the coming weeks. New hospitalizations have also slowly risen during this time period. With higher transmission levels, wearing a mask can prevent individuals from getting sick, testing can help stop the spread of COVID-19, and vaccination with boosting reduces the risk of severe illness and hospitalization.”
Meanwhile, the CDC continues to stress that “healthcare settings should continue to use community transmission rates and continue to follow CDC’s infection prevention and control recommendations for healthcare settings.” The Massachusetts community transmission rates show that all areas of the state, except for Martha’s Vineyard, are considered to have HIGH rates, meaning that new COVID-19 cases per 100,000 persons in the past 7 days are greater than 100 and that the percentage of positive Nucleic Acid Amplification Tests, or NAATs, during the past 7 days are greater than 10%.
House Budget Debate Begins Today
The Massachusetts House will begin debate on the proposed FY2023 state budget the chamber’s Ways & Means Committee recently produced. That proposal generated more than 1,500 amendments last week, including 10 priority amendments from MHA.
MHA’s focus in the amendment process involves, among other priorities, assuring fair reimbursement from the insurance industry, strengthening the behavioral health system and its workforce, expanding telehealth to disenfranchised patient populations who struggle accessing telehealth care, and funding the Health Safety Net at its statutorily required amount.
UMass Memorial Medical Center Receives Foster G. McGaw Recognition
For the third time in recent years, UMass Memorial Medical Center (UMMMC) was selected as one of the top four finalists in the country for the American Hospital Association’s (AHA’s) esteemed Foster G. McGaw Prize.
The prize recognizes healthcare organizations that demonstrate continuous commitment to improving the health and wellbeing for of their communities through efforts addressing health inequities and disparities among populations.
UMMMC was recognized for its community-based response to the COVID-19 pandemic, the hospital’s role within the public health infrastructure, and the commitment and involvement of the system’s CEO, Dr. Eric Dickson, and leadership team in these efforts. In particular, UMMMC’s neighborhood-based strategies to provide vaccines and testing access to at-risk populations and the application of lessons learned to further inform UMass Memorial Health’s ongoing efforts to addressing health equities were recognized. These include redeployment of a Care Mobile team for outreach, and education and testing in neighborhoods using a “Feet on the Street” and Mobile Vaccination Equity Expansion programs. Critical to the success of these programs was use of community-level COVID-19 data, including positivity and vaccination rates. UMMMC’s longstanding, multi-pronged approach to addressing food insecurity, equitable access to healthy foods, and “Food is Medicine” advocacy was also recognized.
The hospital also received Foster G. McGaw recognition in 2019 and 2017. Award recipients each receive $10,000 in funding for community health improvement efforts. The top winner this year was Texas Health Resources, a health system serving North Texas.
MassHealth Extends Postpartum Eligibility
Effective April 1, 2022, MassHealth updated its eligibility policies to provide 12 months of continuous postpartum coverage for those who qualify – up from the previous 60-day coverage period. MassHealth stated that the American Rescue Plan Act (ARPA) gave states the option to extend Medicaid and Children’s Health Insurance Program (CHIP) postpartum coverage from 60 days to 12-months post-pregnancy, which improves access to continuity of care in the critical period after childbirth. MassHealth also said the extension will assist its efforts to address health disparities and advance health equity.
Pregnant members must inform MassHealth of their status to get the expanded benefit. Hospitals often assist the public with the enrollment process; or an individual can visit here.
June 2: Part 2 of the 9th Annual CARe Forum
The next CARe Forum event is scheduled for Thursday, June 2, from 9:30 a.m. to 12 p.m. The CARe Forum is an interactive event that includes testimonials, case study simulations, and group discussions about best practices for communication and resolution programs. Part 1 was held in October 2021 but is not a prerequisite to attending Part 2 in June. The CARe Forum and other work previously done by the Massachusetts Alliance for Communication and Resolution following Medical Injury (MACRMI) are now being led by the Betsy Lehman Center for Patient Safety. Learn more and register here.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association