INSIDE THE ISSUE
> Tabb to Chair MHA Board
> Governor Healey
> Recognizing Excellence & Commitment
> The Hegarty Award
> Racism in Medicine
> Steward’s Uncertain Future
> Endoscopy Policy Paused
> Transition
MONDAY REPORT
Kevin Tabb, M.D. Elected Chair of MHA Board of Trustees
Kevin Tabb, M.D., the president & CEO of Beth Israel Lahey Health, was elected chair of the MHA Board of Trustees last Thursday at the association’s eighty-seventh annual meeting. He succeeds Christine Schuster, R.N., the president & CEO of Emerson Health, and will serve a one-year term.
“Massachusetts has a long, proud history as a hub of healthcare innovation and ground-breaking discovery,” said Tabb. “As chair of the MHA Board, I am honored to partner with leaders across the healthcare landscape to drive positive change for patients, communities, and our dedicated workforce. This year will be another transformative year in healthcare, and together we will work to expand access to high-quality, equitable patient care and advocate for progressive policy solutions that help shape the future.”

He called on the healthcare leaders in attendance to “not just be buffeted by change, but to be agents of that change” to write the next chapter of the state’s healthcare story.
Born in California, Tabb emigrated to Israel at age 18 and served in the Israel Defense Forces. He received his medical degree from the Hebrew University Hadassah Medical School and completed his residency in internal medicine at Hadassah Hospital. Tabb became president and CEO of Beth Israel Deaconess Medical Center in 2011 and in that post helped engineer the 2019 merger of the Beth Israel and Lahey Health systems, which he has since led.
The BILH system is the second largest in the state with 13 hospitals. Last year, BILH and the Dana-Farber Cancer Institute announced a collaboration, pending state approval, that would keep each institution independent but result in a clinical and organizational structure for oncology care, and include construction of a new cancer hospital.
“Dr. Tabb has a bold vision for the future of Massachusetts healthcare, and we know he will help us create an even more innovative and accessible system in the year ahead,” said MHA President and CEO Steve Walsh. “Throughout his career, Dr. Tabb has helped set a national standard on what it means to match outstanding patient care with ingenuity, partnership, and humanity.”
Also at the annual meeting, the following leaders were elected to the board’s membership: Alastair Bell, M.D., CEO of Boston Medical Center Health System; David McCready, CEO of Southcoast Health; Susan Moffatt-Bruce, M.D., president of Lahey Hospital & Medical Center; and Rozanna Penney, president and CEO of Heywood Healthcare.
Michael Dandorph, president & CEO of Tufts Medicine, was elected as the newest member of the board’s Executive Committee. The rest of the Executive Committee for 2024 is Chair Tabb; Chair-Elect Michael Lauf, president & CEO Cape Cod Healthcare; Treasurer Anne Klibanski, M.D., president & CEO, Mass General Brigham; Immediate Past Chair Schuster; Past Chair Most Recently Retired Kevin Churchwell, M.D., president & CEO, Boston Children’s Hospital; and MHA’s Walsh.
Gov. Healey: Healthcare an Essential Part of Massachusetts
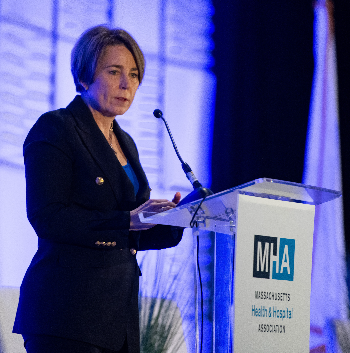
Governor Maura Healey delivered an upbeat address to the MHA Annual Meeting on Friday morning, outlining achievements in workforce, behavioral health, and more her administration in partnership with hospitals and health systems was able to achieve over the last year.
“I want to thank you for your leadership, your persistence, your commitment to making our healthcare organizations a shining example of a more just and inclusive society,” she said. “You also do so at a level of excellence that sets the state apart on the global stage and I take great pride in our Massachusetts healthcare system.”
Calling hospitals “an economic engine in this state” and also “the foundation of our innovation economy,” Healey said it is imperative that state government work closely with the healthcare system “because quite selfishly we can’t afford not to. We as a state cannot afford to see you not succeed.”
Healey Administration filed last week is a provision to make it easier for non-native individuals to become CNAs; the CNA exam will be offered in multiple languages, and the state will cover the cost for first time test takers.
While acknowledging a series of successes, the governor also noted that to continue the state’s path forward it must ease the economic burden on citizens. The administration’s $1 billion tax cut last year benefitted families, she said, but the commonwealth must resolve the pressing housing crisis that is making it unaffordable for many to remain in the state.
The new year will bring additional challenges, both locally and nationally, Healey said, adding on a positive note, “Yeah, there’s stuff happening, but we’re dealing with it.”
MHA Special Recognition: Chief Diversity Officers and Key Legislators
Recognizing the importance of hospital chief diversity and equity officers officers, as well as the legislative leaders whose support is vital to the commonwealth’s healthcare sector, MHA at its annual meeting celebrated the achievements of both.
The equity leaders face the tough task of building support not only within their organizations but also in the community at large as they attempt to diversify the healthcare workforce so that it reflects the populations it serves. Their task has become especially important with the implementation of the Section 1115 Medicaid waiver that embeds health equity efforts at the point of care, makes services more accessible for patients, and reduces persistent disparities.
Pratt Wiley, the president & CEO of The Partnership and an MHA Board of Trustees member, on Friday morning spoke of how the diversity and equity leaders “expertly align equity strategies with business strategies. We see how this community of practitioners, who represent the full ecosystem of our hospital networks from Cape Cod Healthcare to South Shore Hospital to the Brigham and the Farber, UMass Memorial, and all the way to the Berkshires are collaborators who drive innovation both within their organizations and across the commonwealth.”
MHA presented the officers with compasses signifying the direction they provide to the healthcare system.
The night before, MHA presented its Health and Hospital Hero Award to the co-chairs of the legislature’s Joint Committee on Health Care Financing, Sen. Cindy Friedman (D-Arlington) and Rep. John Lawn (D-Watertown).
The award recognizes a public official(s) who has demonstrated outstanding advocacy on behalf of Massachusetts patients and healthcare providers.
MHA President & CEO Steve Walsh said of the honorees, “Through the darkest of times, they made sure our healthcare system had the support and resources it needed to survive. And now that we have entered a new chapter of healthcare, they are at the forefront of public policy that supports our healthcare professionals, breaks down barriers to care, and keeps us at the cutting-edge of patient care. Their fingerprints can be found on every major reform that MHA membership has celebrated over the past few years, including the relief funding that kept our providers afloat during their darkest hour, the support for innovative care models that represent the future of care, and the groundbreaking Mental Health ABC Act that fundamentally changes how behavioral health is prioritized in our state.”
The Hegarty Award: Jim Fanale’s Touching Story
James Fanale, M.D., the former CEO of Care New England and a longtime fixture in Massachusetts healthcare before that, was presented with the Stephen J. Hegarty Memorial Award at MHA’s Annual Meeting.
The award is named after the late Steve Hegarty, who was president of MHA from 1986 to 1995 and a strong advocate for high-quality, accessible healthcare.
Fanale has been battling Stage 4 lung cancer at Dana-Farber Cancer Institute for the past 22 months, and recently wrote about his ordeal in “ONWARD: A Teaching, And A Love Story – For Physicians, And Everyone.” The book focuses on how his perspective changed when he became a patient as opposed to a caregiver.
In his short talk to the attendees, Fanale reminded them that they have “the best job in the world. You get to help people every day. From housekeepers, to physicians, to nurses you can help. So don’t ever forget that as we’re fumbling through the things we have to put up with from compensation to payers, rules, policies, we still get to do something very good every day.”
He told the healthcare leaders in the audience that even though they may be affected by cancer as he has been, “we grew up and work in this system, so we know how to finagle stuff. But imagine those that don’t know where to turn, that don’t have the help or knowledge that others have. The face of cancer, the face of the families – you don’t all see what they’re going through but believe me they go through a lot. I didn’t always realize that,” Fanale said.
Blackstock Addresses Racism on Healthcare
Among the speakers at the annual meeting, Dr. Uché Blackstock firmly held the audience’s attention as she discussed the racism she experienced in the healthcare system, and the importance of diversifying the medical workforce as a step towards removing systemic inequities for patients.
Blackstock, along with her sister Oni and her mother Dr. Dale Gloria Blackstock, were the first mother-daughter legacies from Harvard Medical School.

Her recent memoir Legacy: A Black Physician Reckons With Racism in Medicine takes a critical look at the historical and current state of blacks in medicine and the need for all physicians to offer patients culturally competent care.
Officials Speak Out on Steward’s Uncertain Future
The dire situation of the Steward Health Care system was an unofficial but frequent topic of conversation at the MHA Annual Meeting, as the potential closure or reshaping of the eight current Massachusetts hospitals within the system will have a profound effect on patients, the healthcare workforce, and stability of the entire Massachusetts health ecosystem.
Governor Healey speaking to reporters after her speech at the meeting on Friday said that her administration had not yet seen a firm action plan from Steward. “Our goal is going to be that patients are protected, that jobs are protected, and that the healthcare system in Massachusetts is protected and remains stable,” the governor told reporters.
The Executive Director of the Health Policy Commission (HPC) David Seltz, speaking at the meeting on Friday, was more pointed as he recounted the ongoing legal suit between Steward and the state over the system’s refusal to provide financial data to the HPC and the Center for Health Information and Analysis. All other hospitals in Massachusetts provide volumes of data to the regulatory agencies, as required by statute.
“It’s about having the information so that policymakers and the public can understand the performance of our healthcare system,” Seltz said during a panel discussion. “To me, the obstinate refusal by Steward corporate leadership to hand over these legally mandated reports is a grave disservice to the public, to the patients that are served by that system and to the workers of that system.”
Also on Friday, the Mass General Brigham system said its physicians would no longer be practicing at Steward’s Holy Family campuses, citing concerns about the facility’s ability to meet MGB’s standard of care. That move followed a devastating article in the Boston Globe detailing how a certain medical device was unavailable to staunch bleeding in a young mother at St. Elizabeth’s Medical Center because the manufacturer had repossessed device after Steward had failed to pay its bills. The woman died after giving birth.
BCBSMA Listens to Concerns and Pauses Policy
Blue Cross Blue Shield of Massachusetts (BCBSMA) announced last week that it would delay its plan to enforce restrictions on coverage of monitored anesthesia care (MAC) for colonoscopies and other endoscopy procedures. The insurer’s controversial Medical Policy 154, which went into effect January 1, limited coverage of MAC (or full sedation) for patients with few or no co-morbidities; Blue Cross said such patients could receive less costly moderate sedation administered by a registered nurse.
BCBSMA first announced that it would implement the policy in July 2023 but after facing an outcry from gastroenterology and anesthesiologist societies, as well as physician groups and MHA, the insurer delayed implementation until January 1, 2024. The drumbeat against the ruling continued in recent weeks, with providers arguing that in addition to clinical concerns, the limited-MAC ruling will result in backlogs for colonoscopies at a time when colon cancer rates are rising. The medical community also said Policy 154 would result in a poorer patient experience, reduced efficiency, and the potential to worsen staffing issues because many nurses are not trained to do conscious sedation. Legislators also weighed in with the insurer questioning the policy.
Last week BCBSMA said it would pause enforcement of Medical Policy 154 “until further notice” and would give providers 90-days’ notice prior to it being reinstated. The insurer also said it would do a sweep of any claims that were rejected as a result of the policy to ensure they get properly paid.
“We appreciate Blue Cross’ decision to pause implementation of this policy,” said Karen Granoff, MHA’s senior director of managed care. “We’re especially grateful that no matter our differences, BCBSMA is a local, Massachusetts plan open to dialogue on issues that affect the commonwealth’s healthcare system. That’s not always true of the large national health insurers.”
Transition
Robert Higgins, M.D., is leaving his post as president and CEO of Brigham and Women’s Hospital, and in April will become chief academic officer and president at Rush University in Chicago. He will also serve as senior vice president for the Rush University System for Health. Higgins has led the Brigham since December 2021. Dr. Giles Boland, president of the Brigham and Women’s Physicians Organization and executive vice president at Mass General Brigham, will serve as the hospital’s interim president.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association 