INSIDE THE ISSUE
> Saving $1.75 Billion
> Low Hospital Prices in Mass.
> HPC Cost Trends Hearing
> Within-reach Workforce Solution
> Housing and Health
> HLA Breakfast/NOVA Award
> Transition
MONDAY REPORT
MHA Report: An Important Opportunity for Cost Savings
MHA today released Better Care, Lower Costs: How Massachusetts Can Lead on Sensible Insurance Reform, which identifies an important opportunity to lower healthcare costs in the commonwealth, reduce red-tape obstacles, and re-direct wasteful administrative spending to patient care.
Through a series of recommended actions outlined in the report, as much as $1.75 billion could potentially be saved in the state’s healthcare system that in turn could improve affordability, care access, and delivery of services. The report focuses on three key problem areas and their drivers: wasted resources expended while attempting to reconcile insurance company denied claims; excessive time spent contesting claims denials; and claims processing delays.
New MHA data show that each year 12% of claims that Massachusetts hospitals and health systems file with commercial insurance companies are routinely denied by the insurers – representing $1.5 billion in reimbursement for care services. More than 80% of those denied claims are eventually overturned. The process of “chasing a claim” for approval is expensive and time-consuming, using precious resources that providers could better allocate toward patient care and managing overall costs.
Such delays and denials also affect the financial fragility of hospitals as 42% of Massachusetts commercial insurer claims in hospital accounts receivable (those claims that have yet to be paid) remain, on average, unpaid for 90 days or longer.
“Massachusetts is a leader in innovative cost reform, and we know that every part of the system has a role to play – providers included,” said Michael Sroczynski, MHA’s senior vice president and general counsel. “As our healthcare community grapples with the long-term challenges borne out of the pandemic, reforming insurance practices is an immediate and highly effective way to ease the burden on caregivers and make care more affordable for patients. This is yet another area in which our commonwealth can lead. And we can do it in the here-and-now. We look forward to our continued work with policymakers and partners across the healthcare system in our shared mission to control costs and strengthen our world-class healthcare system for all patients.”
MHA members continue to report that unnecessary “red tape” insurance processes only worsen the pressures brought on by the COVID-19 crisis, including staff burnout, capacity constraints, and patient frustrations. To address these immediate concerns, MHA highlights a set of policy and legislative recommendations that would increase efficiency and reduce costs for patients and providers.
The costs and stresses brought about by certain insurance practices – particularly prior authorizations – have been the subject of increased attention both locally and nationally. In Massachusetts, the Health Policy Commission (HPC), state legislators, and a coalition of healthcare providers and advocates are leading the charge to reduce administrative burdens. Prior authorization disputes and excessive documentation requirements, among other insurance-related administrative burdens, are also a major cause of burnout in the healthcare profession. The HPC’s annual cost trends hearing this week (see related story below) is expected to touch on some of the issues cited in the MHA report.
Mass. Hospital Prices Relative to Medicare Among Lowest in Country
In the Health Policy Commission’s (HPC’s) 2023 Annual Cost Trends report that is the focus of a hearing this week, the HPC identifies “excessively high prices” of healthcare providers as one of the areas contributing to the growth in healthcare costs. However, the most recent RAND Corporation study of commercial spending for hospital services – a resource the HPC frequently cites – shows that Massachusetts has among the lowest hospital commercial prices relative to Medicare in the country.
RAND’s Prices Paid to Hospitals by Private Health Plans – Findings from Round 4 of an Employer-Led Transparency Initiative is based on an analysis of more than 4,000 hospitals in all states from 2018 to 2020. Using Medicare’s grouping and pricing methodologies, RAND repriced claims for hospital services that private insurers pay for, and then compared the repriced services to the actual payments the private insurers make.
For the nation, RAND found employers and private insurers paid 224% of what Medicare would have paid for the same services at the same facilities. RAND reports the median relative price across all states was 248%.
But for Massachusetts hospitals, RAND found commercial payers paid 179% of Medicare prices for hospital services. The study found the commercial-to-Medicare relative price ratio for Massachusetts inpatient and outpatient services was consistently low – or 178% and 180% respectively.
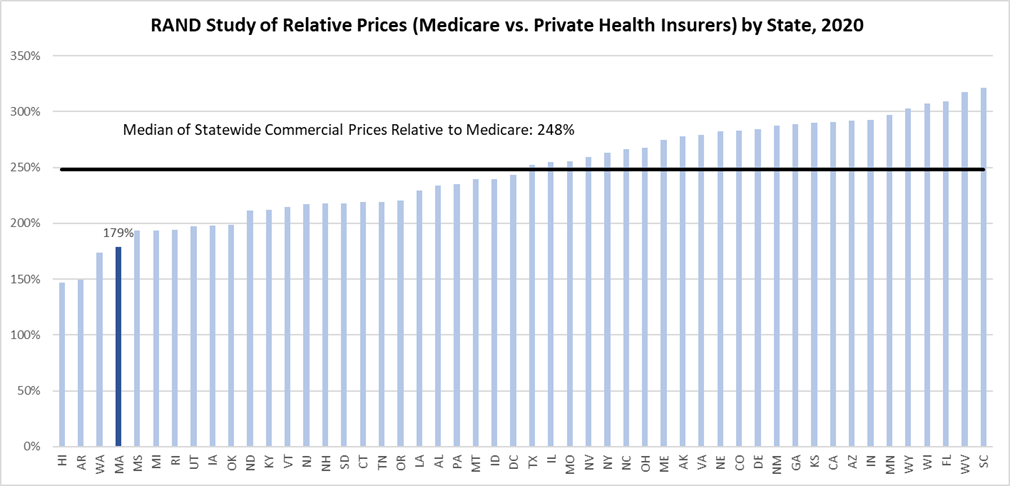
In its 2023 Annual Cost Trends Report, the HPC provided an analysis that compared Massachusetts commercial spending on key healthcare services to Medicare and MassHealth (Medicaid) reimbursement, identifying the portion of spending that exceeded 200% of that Medicare and MassHealth reimbursement. While commercial prices for hospital services exceeds Medicare in all states, the RAND price transparency report shows the Massachusetts experience is anything but excessive. According to RAND, Massachusetts ranked 47 out of 50 states for commercial hospital prices relative to Medicare pricing. Notably, the RAND study solely uses Medicare as its benchmark for comparing hospital payment, whereas the recent HPC analysis used MassHealth reimbursement when evaluating whether commercial payer prices for inpatient hospital services were excessive. MassHealth inpatient reimbursement is significantly lower than inpatient Medicare rates.
MHA’s Vice President of Healthcare Finance and Policy Dan McHale said, “The RAND report is yet another indicator of the progress that has been made in Massachusetts to control healthcare costs, especially in context with the rest of the nation. Massachusetts hospitals and health system providers continue to be focused on finding ways to make healthcare more affordable while balancing the need to support their workforce and make investments in their facilities to ensure high-quality care remains accessible for all.”
HPC Holds Cost Trends Hearing on Wednesday
The Health Policy Commission’s (HPC’s) Annual Cost Trends hearing this Wednesday, November 8 comes at a time when the hospital and healthcare community is still in search of long-term solutions to reverse the negative financial and operational trends adversely affecting the system.
In addition to the well-documented problems affecting providers – including unprecedented workforce shortages that are causing hospitals and health systems alone to spend more than $1.5 billion annually on temporary clinical staffing – the system is facing other input costs beyond its control. Increased costs of fuel, supplies, transportation, and other inputs that all other economic sectors are facing are also burdening the healthcare sector. But while other sectors often quickly pass those costs on to consumers, providers cannot. Providers are locked into contracts with their payers – both public payers and commercial health insurance companies. And as the finances of hospitals and health systems continue to be weak following a devastating FY2022; the state reports that 71% of hospital health systems experienced negative operating margins through the third quarter of FY2023.
Most hospitals are at full capacity during this time of reduced staff, and the threat of even more patients coming through their doors increases as the flu/RSV/COVID-19 season encroaches.
All the while, healthcare providers continue their longstanding efforts to limit cost growth. Those efforts include reducing the use of low-value services, expanding value-based care, and adopting innovative and efficient care models – such as telehealth and hospital at Home. At Wednesday’s hearing, hospital CEOs are expected to reiterate their commitment to making care more affordable for the patients they serve, even as the system struggles.
MHA this week identified a $1.75 billion savings opportunity related to administrative expenses, which would not negatively affect access to medical services (see related story above). Other cost-cutting efforts that are within the HPC’s control involve investigating and addressing spiraling pharmaceutical costs – over which providers have little control – and attempting to rein in the pernicious influence of pharmacy benefit managers (PBMs) in those drug costs.
“World-class healthcare means care that is affordable – there is no question,” said Steve Walsh, MHA’s president and CEO. “But the commonwealth simply cannot meet our cost goals until we have solved the biggest pressures facing providers: workforce shortages, unrelenting capacity issues, and dire financial losses. This is our moment to be bold. We can cut the red tape. We can fully empower care innovation. And we can make sure every component of the system is at the table with the same mission in mind. All of these things not only reduce costs; they are better for patient care. MHA and our members look forward to working with the HPC and our partners with this mission in mind.”
Key Hearing This Week on Oft-Delayed Workforce Solution
The Joint Committee on Health Care Financing’s hearing tomorrow, November 7, will consider legislation that would authorize Massachusetts to join 41 states and jurisdictions that have adopted the national Nurse Licensure Compact (NLC).
The NLC – endorsed widely by hospitals, nurse leaders, the Health Policy Commission, patient advocacy groups, and even the Boston Globe editorial board, among others – has been hung up on Beacon Hill for years. The Compact’s simple premise – allowing qualified nurses to have one license in their state of residency and to practice in other NLC states – makes sense for a lot of reasons, especially in the post-pandemic environment.
H.1211/S.747, An Act Relative to Nurse Licensure Compact in Massachusetts from Rep. Kay Khan (D-Newton) and Sen. Barry Finegold (D-Andover) would allow Massachusetts to finally join the national compact after several legislative sessions of deliberations on the issue. Nurses participating in the compact would be required to go through strict criminal history reviews and they would have to meet all the licensing requirements of the states in which they wanted to practice.
“The NLC does not pose an elevated risk to patient safety or place an additional burden on states in terms of discipline case management,” the National Council of State Boards of Nursing found in a 2022 study. “Multistate license holders not only increase access to care across NLC state lines, when necessary, but they also maintain and augment patient safety.”
Patients pour into Massachusetts from surrounding states seeking the commonwealth’s world-class care and the state’s protected access to reproductive services, abortion services, and gender-affirming care. The NLC would permit Massachusetts nurses to use telehealth to provide follow-up care for those patients who then return to their home state. It would allow all nurses to pick and choose shifts across state lines, providing them with the flexibility that many of them are seeking post-pandemic. And because the pool of nurses is widened, hospitals – acute care facilities as well as post-acutes – will not have to rely as much on expensive travel agencies to fill vacancies.
An MHA study showed that there were an estimated 5,100 R.N. vacancies at Massachusetts hospitals in 2022, and that hospitals are spending more than $1.5 billion annually to fill vacant posts through use of travel agencies.
A researcher who is often quoted in nursing-related issues, Linda Aiken from the University of Pennsylvania, said in September after Pennsylvania joining the NLC, “This is a great thing. It takes away the bureaucratic delay. There is not a strong rationale for having all these separate licenses.”
In 2021, the HPC studied the issue and closely and determined that “Compact membership would enhance the ability of the Massachusetts healthcare system to prepare for pandemics, emergencies, and other staffing needs and to facilitate telehealth and other care delivery transformations in the future. … There is no evidence that joining the NLC would have a negative effect on quality of nursing care in the commonwealth and the ability to fill short-term staffing needs and facilitate telehealth could yield positive effects for healthcare access, quality, and cost.”
“There’s an urgency to this issue,” said Amanda Stefancyk Oberlies, R.N., the CEO of the Organization of Nurse Leaders – MA, RI, NH, CT, VT. “The healthcare system is working around the clock to boost its workforce, and this is a proven solution that is right at our fingertips. We need to make Massachusetts a Compact state as soon as possible to relieve the pressure on R.N.s and to improve care access for patients. It’s time for the commonwealth to catch up with the rest of the nation and embrace this workforce-friendly care innovation.”
The Link Between Housing and Health
A recent report from the Green & Healthy Homes Initiative (GHHI) provides solid data to show how a community’s housing stock can affect health outcomes for its citizens.
GHHI focused on three Massachusetts Gateway Cities – Brockton, Holyoke, and Springfield – and found that they have a higher proportion of housing units with lead paint compared to statewide averages. The communities also have a higher-than-average rate of confirmed child elevated blood lead levels (EBLLs), as well as higher rates of asthma, which can be an indicator of poor indoor air quality. Another indicator of poor air quality – chronic obstructive pulmonary disease (COPD) – also occurs in Brockton, Holyoke, and Springfield at higher rates than the rest of the state.

“Due to historical patterns such as racial segregation and redlining, communities of color have been underinvested in compared to white communities, and therefore are more likely to face problems with housing quality,” GHHI writes. “Additionally, by virtue of low-income communities having fewer resources to remediate housing quality issues, low-income communities also are more likely to have housing quality issues that impact health.”
The report was prepared for the Massachusetts Association of Community Development Corporations (MACDC).
MassINC defines “Gateway Cities” as “midsize urban centers that anchor regional economies around the state.” They previously contained industries that were considered “gateways” to the American Dream but have since faced “stubborn social and economic challenges” while retaining ” unrealized potential.” The original 11 gateway cities were Brockton, Fall River, Fitchburg, Haverhill, Holyoke, Lawrence, Lowell, New Bedford, Pittsfield, Springfield, and Worcester. The legislature in 2009 and 2010 added Attleboro, Barnstable, Chelsea, Chicopee, Everett, Leominster, Lynn, Malden, Methuen, Peabody, Quincy, Revere, Salem, Taunton, and Westfield.
Hospitals in Massachusetts have recognized the link between housing and health and it is an important component of many community benefit programs. And the state’s MassHealth 1115 waiver includes provision to track and reward asthma remediation programs. GHHI’s report contains a series of further recommendations to address the issue.
Mark Your Calendars
Health Law Advocates (HLA) is holding its Twenty-Eighth Annual Benefit Breakfast on Friday, November 17 at the Sheraton Boston Hotel, with coffee hour beginning at 7 a.m., followed by the main event from 8 to 9:15 a.m. The breakfast features a talk by writer Min Jin Lee whose novel Pachinko was a finalist for the National Book Award. Register here.
The American Hospital Association (AHA) Dick Davidson NOVA Award celebrates AHA members for programs that improve community health status through healthcare, economic or social initiatives; are collaborative with community organizations and/or other hospitals and systems; and engage community members in identifying and co-designing solutions or interventions. Five organizations will be recognized with the award. Applications are due November 13.
Transition
Abha Agrawal, M.D., is the new president and CEO of Lawrence General Hospital, effective January 2024. Agrawal is a practicing internal medicine physician, clinical informaticist, and author currently serving as CMO at Humboldt Park Health in Chicago. She is also the founder of A4 Clinics in India, which are neuro rehabilitation centers. Agrawal’s appointment culminates a six-month search process, during which the hospital was led by Interim CEO Robin Hynds, who will resume her role as Lawrence General’s EVP and COO in January. Agrawal is a graduate of S.N. Medical College in Agra, India. She completed a fellowship in medical informatics at Yale University School of Medicine, and was resident and chief resident at SUNY Downstate Medical Center and SUNY Health Science Center at Brooklyn. She received a Fulbright Award in India.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association 