Medicaid on the Chopping Block

INSIDE THE ISSUE
> Rep. Clark on Medicaid Cuts
> Hospitals on Need for MassHealth
> Healey on NIH/Medicaid
> Neal’s Commitment
> Transition
MONDAY REPORT
Medicaid on Chopping Block to Meet Budget Goals
As the federal budget process moves forward under the Trump Administration’s stated goals of dramatically reducing government funding and taxes, attention has been focused on where government cuts will occur to make up for the lost revenue from the tax cuts.
The blueprints for the budget process are the House and Senate budget resolutions that passed in February; the House version proposes that the House Energy and Commerce Committee find $880 billion in cuts over the next decade. According to the Congressional Budget Office, Medicaid comprises 93% of the federal programs, excluding Medicare Part B, under the purview of Energy & Commerce. (The CHIP program – Children’s Health Insurance Program – accounts for another 2%.)
So to meet House Republican budget cutting goals, if they are finalized in a final budget resolution, Medicaid would somehow be affected. President Trump and House Speaker Mike Johnson (R-La.) have said the Medicaid cuts will focus only on the broad terms “fraud and abuse.”
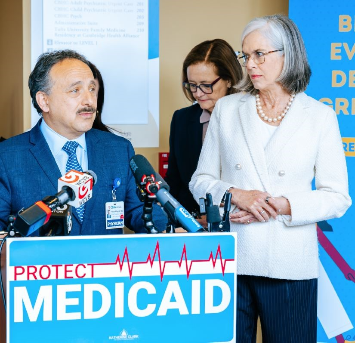
Last week, Representative Katherine Clark (D-Mass.), the Democratic Minority Whip, organized a roundtable and press conference at Cambridge Health Alliance’s (CHA’s) Malden Care Center to call attention to what is at risk from Medicaid cuts. Joining Clark were Massachusetts Health and Human Services Secretary Kate Walsh, Cambridge Health Alliance CEO Dr. Assaad Sayah, MHA’s Vice President of Government Advocacy and Public Policy Emily Dulong, Traci Brooks, M.D., CHA’s chief of pediatrics, and a local patient advocate.
“The only way you get the $880 billion that they are going to take out of the system is through Medicaid,” Clark said of the Republican majorities in the House and Senate. “They’ve written it down. They voted on it. They’re pursuing it, and they are doing it with the full blessing of the Trump administration.”
CHA’s Sayah said that Medicaid is “absolutely critical” to the health system’s mission, “which is to care for the communities we serve and the patients who truly rely on us everyday – not only for their healthcare but for everything we provide to them. We’re involved in their social determinants [of health]. We care for them physically, mentally, psychologically; we care for their families and their communities, and Medicaid is absolutely an integral part of this work.”
MHA’s Dulong noted that Medicaid is an essential component of the entire Massachusetts healthcare system and its mission of delivering high-quality care.
“This fundamental mission becomes impossible to meet without adequate Medicaid funding,” Dulong said. “Massachusetts leaders understood this when in 2006, they came together to enact the landmark law to expand access to health insurance coverage for all our neighbors. Our Medicaid program is the foundation that our communities and our entire healthcare system are built upon; it is what truly makes Massachusetts not just a state, but a commonwealth.”
For some Massachusetts hospitals, upwards of 75 to 80% of their patients are publicly insured or uninsured. “Medicaid is what helps keep their doors open,” Dulong said. “It is so deeply engrained in their institutions’ budgets, and makes the provision of care possible for all of their patients.”
MHA Asked Its Members: What’s Medicaid Mean to You?
In Massachusetts, about 2.1 million people or 30% of the population, are covered through the state’s Medicaid program – MassHealth.
Nearly half of all children are covered by the program and 59% of people with disabilities are on Medicaid. Almost all Massachusetts hospitals derive the bulk of their revenue from public healthcare programs – Medicaid and Medicare – with the remaining revenue coming from private health insurance.
Many people who would lose MassHealth coverage through potential cuts could become uninsured. When the uninsured become ill, they will often defer care because they can’t afford treatment, or their sickness will progress to the point where they show up in hospital EDs, requiring more and expensive services than they would have if they sought treatment earlier.
Such uninsured care is paid for by the Health Safety Net, which is already facing a projected $200-plus million deficit, meaning hospitals must absorb the cost on their own. In turn, commercial insurance premiums could increase further, driving up the cost of care for everyone.
MHA asked its membership recently how the theory of Medicaid cuts manifests itself in the real world. Here’s what some hospitals and health systems said.
Baystate Health
Baystate Health is already in the midst of a $225-plus million core operations transformation and are turning over every stone with respect to workforce, supply chain, revenue cycle, clinical operations, physician enterprise, and strategic growth. Today, Medicare and Medicaid represent more than 70% of our patient population. On top of the existing transformation workstreams, we would have to consider additional radical steps to, at a minimum, move towards Medicare profitability to make up for additional underpayment for Medicaid. These drastic moves could include exiting unprofitable service lines, reducing teaching and research, minimizing physician enterprise investments, or downsizing our workforce – with the understanding that we are the major employer and economic pillar in Western Massachusetts.

Hebrew SeniorLife
Since 1993, Hebrew SeniorLife’s Hebrew Rehabilitation Center (HRC), licensed in Massachusetts as a Chronic Disease and Rehabilitation Hospital, has demonstrated successful collaboration with Medicaid to provide high-quality services to underserved, frail older adults by managing and coordinating overall care, improving quality of life, and lowering the cost of care. Hebrew Rehabilitation Center serves more than 700 Medicaid members annually.
These patients have complex chronic diseases that require a unique long-term chronic care setting. They receive high-quality services, including complex wound care, dialysis, chronic tracheostomy care, blood product transfusion, intensive palliative care, and intensive behavioral health services. HRC has two bilingual floors for Russian-speaking patients and three floors of intensive memory support to meet the complex needs of patients.
Approximately 75% of patients at Hebrew Rehabilitation Center are on MassHealth. Therefore, approximately 80% of the Hebrew Rehabilitation Center’s revenue relies on Medicaid and Medicare. These payers are critical to the operations of this safety-net long-term chronic care hospital.

Saint Anne’s Hospital (Brown University Health System)
Medicaid funding is critical to both Saint Anne’s Hospital and the patients it serves. The average household income in Fall River is approximately $53,000, with nearly 21% of Greater Fall River area household incomes below the poverty line. In addition, the incidence of chronic diseases, such as diabetes, stroke, hypertension, and chronic obstructive pulmonary disease exceeds Massachusetts state averages. More than 26% of Saint Anne’s patients currently rely on Medicaid to pay for their care.
A significant number of Saint Anne’s patients who rely on Medicaid are served by our Fernandes Center for Children & Families, which provides a unique model of care for coordinated ambulatory evaluations, diagnosis, and treatment services to children with special healthcare needs, including complex medical problems, developmental disabilities, behavioral health, and chronic diseases. It is the only such facility that accepts Medicaid in the Greater Fall River area. In FY2024, more than 74% of the center’s patients were enrolled in Medicaid.
As part of its mission, Saint Anne’s also provides health insurance screening and enrollment assistance to patients and community members. In FY2024, the hospital screened and/or enrolled 2,976 individuals in health insurance. Overall, St. Anne’s maintains a greater than 90% success rate in completing Medicaid applications for otherwise uninsured or self-pay patients.
Significant Medicaid cuts would have dire consequences for the patients and communities that Saint Anne’s Hospital is proud to serve.
Healey at Children’s: Don’t Gut NIH and Medicaid Funding
In addition to potential Medicaid cuts, the Trump Administration has made it clear that National Institutes of Health (NIH) funding will not be exempt from budget reductions.
Massachusetts has consistently ranked among the top states in the nation receiving NIH funds, which is a reflection of the commonwealth’s preeminence in healthcare, higher education, and the life sciences.
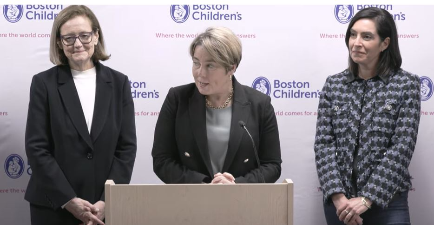
Last week, Governor Maura Healey, her partner Joanna Lydgate, and Health and Human Services Secretary Kate Walsh were hosted at Boston Children’s Hospital by the facility’s CEO Dr. Kevin Churchwell.
“Right now, the Trump Administration and Congressional Republicans are trying to gut NIH and Medicaid funding, which would take away healthcare from babies, pregnant women, seniors, and people with disabilities and halt clinical trials at Boston Children’s and institutions across the state,” Healey said. “These actions will have real harm on the health and wellbeing of our children and will prevent doctors and researchers from doing their jobs.”
Walsh noted that nearly half of all children in the commonwealth rely on MassHealth or CHIP. She added, “Cuts to funding for things like medical research and grants for graduate medical education at children’s hospitals are really creating a no-win situation, not only impacting research teams but harming our Massachusetts economy (which is a net contributor to the federal budget), undermining the US’s world leadership in medical research, and depriving patients and families of life-saving innovations.”
Boston Children’s is a leading recipient of pediatric research funding from the National Institutes of Health. Approximately 46% of Boston Children’s patients are covered by MassHealth, including 60% of patients with the most complex medical needs.
Neal Visits Easthampton Facility to Discuss Medicaid

Medicaid isn’t just for patients in nursing homes and hospitals. Those receiving services through agencies like Riverside Industries in Easthampton also benefit from the public payer program.
Riverside Industries since 1968 has provided individualized services combining life skill development, day habilitation, and employment options for adults living with intellectual and developmental disabilities in Western Massachusetts.
Last week, Rep. Richard Neal (D-Mass.), the ranking member on the House Ways & Means Committee, visited the facility to discuss how Medicaid cuts would hurt Riverside and the patients it serves.
“After receiving more than 150 letters from men and women who rely on Medicaid to receive those services, I visited them to deliver this message: we will continue fighting for them and against any attempts to cut the critical lifeline of care and coverage that Medicaid provides,” Neal said last Wednesday.
Transitions
Diana Richardson has been named interim president and CEO of the Lawrence General Hospital and Holy Family healthcare system. She fills the vacancy left by the February resignation of former CEO Dr. Abha Agrawal. Richardson most recently served as senior transition liaison with the Massachusetts Department of Public Health, where she was instrumental in the state’s response to the Steward Health Care bankruptcy. Before DPH, Richardson served as president of Tufts Medical Center in Boston from October 2022 to March 2024. She is a graduate of Boston University and holds an MBA from Bentley University. The system said a national search is underway for a permanent CEO.
South Shore Health has named Sam Skura as its executive vice president and COO. Skura will oversee all clinical, administrative, and support service, operations among the system’s 6,500 employees, according to the South Shore announcement. Skura, a former MHA Trustee, previously served as the president of Baystate Medical Center and senior vice president of operations for the Baystate system. He has also served as COO at Beth Israel Deaconess Medical Center and vice president of clinical operations at Lahey Hospital and Medical Center.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association