PLEASE NOTE: MHA has upgraded its Member Portal. Click here to gain access.
New Vaccine Policy; Beautiful Bill Not So Pretty

INSIDE THE ISSUE
> Detailing Coverage Losses
> New Mass. Vaccine Policy
> Unity for Change
> Important BH Hearing
> Transition: Sroczynski to Lead HARI
MONDAY REPORT
New Report: “Beautiful” Bill Leads to Loss of Coverage
The Blue Cross and Blue Shield Foundation, using a model developed by the Urban Institute, has attempted to specifically quantify how the recently passed “One Great Beautiful Bill” (OB3) will affect health insurance coverage in Massachusetts in the future.
According to the Foundation’s report, two of OB3’s provisions – mandatory six-month redeterminations and work reporting requirements – will result in between 141,000 and 203,000 MassHealth members losing coverage. That translates into the current number of uninsured individuals in Massachusetts increasing by more than 50%. Other Medicaid and marketplace provisions in OB3, which were not covered in the report, could lead to even further coverage losses, according to the Foundation.
The commonwealth’s Health Safety Net program, a key element of financing care for the uninsured, is already facing record breaking financial deficiencies before factoring in these new projections.
Under the new law, by December 31, 2026, states must redetermine eligibility for certain Medicaid members every six months, instead of every 12 months. The work reporting provision of the bill requires, by January 1, 2027, certain adults to show they have participated in qualifying activities (work program, community service, part-time education) at least 80 hours per month in order to be eligible for Medicaid.
Using the Urban Institute model, the Blue Cross Foundation found that some people losing coverage would enroll in employer sponsored coverage, and some could be eligible for subsidized Health Connector coverage. But the vast majority – 110,000 to 180,000 – would remain uninsured over the course of the year.
The OB3 redetermination and work reporting requirements have been criticized mainly because of the large administrative burdens they impose on individuals and states.
“Overall, these two policies are likely to cause many MassHealth members to be procedurally terminated,” according to the report. “In other words, many people will lose coverage because they aren’t able to verify their eligibility – not because they are no longer eligible. Overall, of those losing coverage because of the work reporting requirement, it is likely that many would, in fact, be exempt or compliant. We cannot assess the exact share with certainty. Many people would have to verify their compliance or exemption because it would not be possible for the state to verify their compliance or exemption using existing data sources. In all three states that have implemented work requirements—Arkansas, New Hampshire, and Michigan— disenrollment was largely driven by members’ non-response to notices asking them to verify their compliance or exemption, suggesting people were unaware of reporting requirements … In addition to being harmful to those whose coverage is interrupted, this churn in enrollment also increases Medicaid program costs.”
Many people in Massachusetts who lose coverage and need care will rely on the Health Safety Net, which is running a $290 million deficit this fiscal year (ending on September 30) and, without funding relief, is projected to run even larger deficits once the OB3 provisions take effect. Hospitals alone are responsible for covering any Health Safety Net shortfall, placing a serious strain on their operational and financial stability. MHA has been working closely with the Healey-Driscoll administration and the legislature to explore legislation that can help mitigate the financial losses in the safety net ahead of a rapidly approaching deadline.
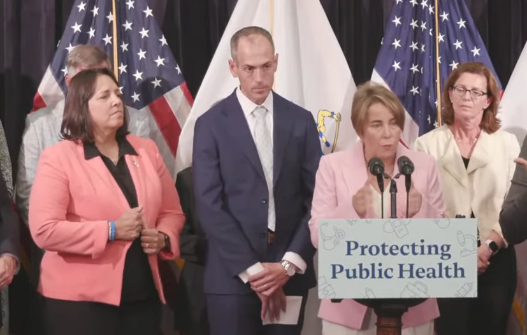
Decrying Federal Inaction, Healey Shifts Vaccine Decisions to State
Massachusetts has made it easier for pharmacies in the state to provide COVID-19 vaccines to a wide swarth of the population, and has shifted the vaccine recommendation process from the federal government to the state’s Department of Public Health.
Massachusetts was among 16 states that required the Centers for Disease Control and Prevention (CDC) to sign off on a vaccine before pharmacies in the state could administer it. Because of the current disarray at the CDC, and U.S. Health and Human Services Secretary Robert Kennedy’s dismissal of many pro-vaccine members of the Advisory Committee on Immunization Practices (ACIP), it became clear that states relying on federal government sign off before vaccines became available to their residents was problematic.
In August, the Food and Drug Administration recommended providing the latest COVID-19 vaccine only to those over age 65 with specific medical conditions. ACIP will meet on September 18 and is expected to approve the FDA recommendation. That means that many people, including children, will no longer have easy access to the COVID-19 vaccine as they have since 2020.
But last week, Massachusetts announced a standing order, signed by DPH Commissioner Robbie Goldstein, M.D., that authorizes qualified pharmacy personnel to dispense and administer the COVID-19 vaccine in Massachusetts to all eligible persons, which includes – depending on the brand of vaccine – anyone over age 5. Last week, Governor Maura Healey also announced that insured commercial health plans in Massachusetts, along with MassHealth and the Group Insurance Commission, will continue to cover vaccines that DPH recommends, regardless of what any other agency or official may say. That directive covers not just COVID and flu shots, but also childhood vaccines, such as those for mumps and rubella. The state also released guidance authorizing qualified pharmacy personnel to administer certain vaccines as designated by DPH.
“We believe healthcare is a right and public health is a responsibility,” Healey said at a Thursday press conference announcing the changes. She said Massachusetts would form a collaboration with other Northeast states to coordinate public health responses, such as attempting to reach consensus on vaccine recommendations and protecting state labs, as well as joint disease monitoring and emergency response.
“Wherever the federal government has created a devastating and harmful gap we will look to do everything we can to protect the public health of residents in Massachusetts, and work with our sister states to stand up and protect the public health of Americans,” Healey said.
Commissioner Goldstein said in the coming weeks he will use data from the Vaccine Integrity Project and consult with professional groups such as the American Academy of Pediatrics and the American College of Physicians to help him arrive at vaccine recommendations for Massachusetts.
“Vaccines are the greatest public health advance of our time,” Goldstein said.
Diverse Health Groups Call for Unity to Bring About Change
A health insurance company executive and leaders of the groups representing hospitals, community health centers, and patients joined to craft an op-ed calling for unity and resolve to protect the “state’s world-class healthcare ecosystem.”
The op-ed – “Collaboration is crucial to save healthcare in Mass.” – ran in the August 30 issue of The Boston Globe. It was signed by Michael Curry, the president and CEO of the Massachusetts League of Community Health Centers; Manny Lopes, the president and CEO of Fallon Health; Amy Rosenthal, executive director of Health Care For All; and MHA President & CEO Steve Walsh.
Noting that the “chaos” emanating from Washington. D.C. has further affected the state’s troubled healthcare system, the health leaders wrote, “Chaos breeds division, and we are seeing battle lines being drawn across the country when it comes to what we value and where dollars are spent. But healthcare is inherently a team sport. It cannot operate in divided silos. As representatives of local patients, hospitals, health systems, health plans, and community health centers, we are calling for a new era of collaboration among the state’s most trusted, longtime health care stakeholders.”
The leaders, citing “public squabbles and distractions that have defined local policy conversations,” specifically called for unity on such initiatives as building the healthcare workforce, lowering prescription costs, modernizing and reinvesting in MassHealth, supporting telehealth and Hospital at Home, and investing and embracing AI “as a transformative tool to enhance care delivery, streamline operations, and empower both providers and patients.”
Building on Behavioral Health Success
Tomorrow, September 9, the Joint Committee on Financial Services will hold a hearing on MHA priority legislation – H.1131/S.773, An Act Expanding Access to Mental Health Services, sponsored by Rep. Marjorie Decker (D-Cambridge) and Sen. John Keenan (D-Quincy).
The legislation builds upon the comprehensive Addressing Barriers to Care or ABC Act (Chapter 177 of the Acts of 2022), which, among other things, increased equitable reimbursement for mental health providers and addressed hospital emergency room boarding through real-time bed availability data.
The proposed law being heard tomorrow would ensure commercial health insurance coverage of certain behavioral health services, including commercial coverage for behavioral health evaluations performed in emergency departments. Importantly, the proposed law would improve access to behavioral health services by expanding the number of behavioral health settings that must be covered without prior authorization. The legislation also aligns the approval process for psychiatric units in acute care hospitals with the approval process for freestanding psychiatric facilities. It would waive application fees for mobile integrated health services that have a behavioral health focus, and aligns coverage requirements of behavioral health crisis services required in Chapter 177 with how these services are delivered after the changes made by the Roadmap for Behavioral Health Reform.
“The commonwealth has previously taken bold action to improve the behavioral health system,” said Leigh Simons, MHA’s senior director, healthcare policy. “This proposal builds on that record of achievement by taking additional measured steps to expand care access while promoting fair payments and shared responsibility for those caring for behavioral health patients and their families.
Transition: Sroczynski to Lead HARI
Mike Sroczynski, who most recently served as MHA’s executive vice president and general counsel, has been named the president of the Hospital Association of Rhode Island (HARI), effective last Tuesday. He succeeds Howard Dulude, who had served as the organization’s interim president since August 2024. As president, Sroczynski will lead state and federal advocacy efforts, convene healthcare leaders, and advance the organization’s mission on behalf of its 17 hospital and health system members. Sroczynski first began working at MHA in 1999, and has developed a reputation as one of the most visible, effective advocates for healthcare providers in the region over those 25 years.
“Rhode Island is home to a special healthcare community with deep roots in neighborhoods and even deeper ambitions for the future of patient care,” Sroczynski said. “I am honored to help uplift the voices of our hospitals and health systems at a time when provider voices are needed the most.”
Sroczynski, who graduated from Syracuse University’s Martin J. Whitman School of Management and College of Law, will continue to serve as MHA’s general counsel.


 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association