Research, More OB3 Bad News, New System Name

INSIDE THE ISSUE
> DRIVE Initiative
> Healey “Lean Into” HSN Funding
> More OB3 Bad News
> Merrimack Health
> DSH Cuts
> Preceptorship Tax Credit
> Supported Decision-Making Agreements
> Concern With 340B Rebates
MONDAY REPORT
Healey Urges Quick Passage of DRIVE Initiative
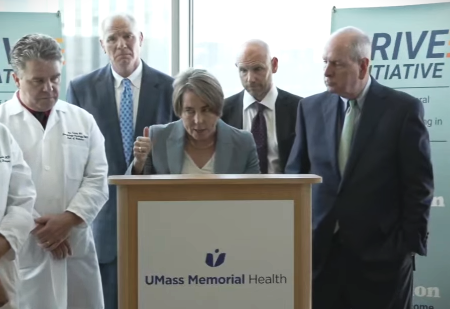
About a month and a half after introducing her DRIVE legislation, Governor Maura Healey was on the road last week, promoting the initiative in Worcester, and urging its quick passage.
DRIVE stands for “Discovery, Research and Innovation for a Vibrant Economy,” consisting of a $200 million research funding pool housed at MassDevelopment, and another $200 million for public higher education campuses to support direct and indirect costs of research, cross-regional partnerships, joint ventures, and to preserve and hire positions in research and teaching. Half of the funding would come from the so-called “Millionaire’s Tax” and the other half from interest off the state’s stabilization fund.
“Research funding means jobs, growth, it means a better economy,” Healey said at a press conference held at UMass Memorial Medical Center. The governor first announced the DRIVE initiative at the end of July, noting at the time that the measure was not just a response to the Trump administration’s cuts to federal research funding, but also as a way for Massachusetts to preserve its medical research ecosystem and create jobs.
Last Wednesday at UMass, Healey said DRIVE and its timely passage is a priority for her administration. “Anything that puts a pause on research, means we end up losing decades of results” in curing disease and giving hope to patients, she said.
“This amazing ecosystem is in trouble if we don’t find some way to keep it going,” said Eric Dickson, M.D., the president & CEO of UMass Memorial Health and a member of the MHA Board of Trustees.
Michael Collins, M.D., the chancellor at UMass Chan Medical School, praised the DRIVE initiative and Healey’s commitment to science. “The science that is being done today are the Nobel Prize discoveries of 20 or 30 years from now,” Collins said. “Now is the time for us to be doubling down on research.”
Healey: Research is Key, But So is Safety Net Funding
Governor Healey was gung-ho on her DRIVE initiative last Wednesday, noting that the collection of healthcare interests coming together with academic, life science companies, state government, and others to create groundbreaking medical advances “is not happening like this in every state, or every country.”
But when asked what else needs to be done to stabilize that ecosystem in the face of ongoing federal cuts, Healey was quick to point out the need to stabilize the Health Safety Net – the fund that pays providers for the care they provide to uninsured and underinsured individuals. As has been reported extensively in Monday Report, the fund is facing record shortfalls (see story below), which are covered solely by hospitals. The number of uninsured in the state is expected to rise due to the provisions contained in the recently passed One Big Beautiful Bill (OB3).
“[T]he other thing that is important for the legislature to act on is shoring up the Health Safety Net,” she said in response to a reporter’s question. “We need to make sure that facilities like UMass Memorial, which are the safety net hospitals for central Massachusetts, have the funding they need to enable people to continue to access care. And yes, the Trump administration made it a heck of a lot harder through the Big Beautiful Bill and Congress that is taking away funding for hospitals and healthcare centers. So that’s why it’s important that we act quickly in this state to shore up our healthcare delivery system – and I’m going to continue to work on and lean into that.”
MTF Report on OB3: Health Safety Net Under Threat
The evidence keeps building about how the One Big Beautiful Bill (OB3) will most likely harm Massachusetts healthcare and the patients it serves.
First, the bipartisan Congressional Budget Office (CBO) detailed how many millions nationwide would lose coverage. This month the Blue Cross Blue Shield Foundation calculated that up to 203,000 people in Massachusetts alone would lose their insurance. Now the Massachusetts Taxpayers Foundation (MTF) has issued a report detailing how OB3’s healthcare provisions will affect Massachusetts finances, all of which could further challenge patient care.
MTF estimates that 255,000 people in Massachusetts will lose coverage over the next 10 years due to OB3, and that federal health care spending in the state will be reduced by $1.8 billion per year, as Health Safety Net demand increases by $510 million.
Specifically, MTF found that OB3 will require the state to spend more on administrative costs to track the bill’s Medicaid work requirement provisions. While those work requirements will most likely reduce Medicaid enrollees, and hence MassHealth expenditures, the decrease will also result in less federal matching funds flowing to Massachusetts and, most importantly, an increase in the uninsured rate as the CBO and Blue Cross reports have noted.
“An increase in the uninsured population will increase financial pressure on the state’s larger health care system, as the cost of care for uninsured residents is covered through the state’s Health Safety Net, which currently has a funding shortfall of approximately $290 million and reimburses providers at rates far below MassHealth,” MTF writes in its timely report.
“MTF’s report illustrates the profound disruptions our state’s healthcare system will be forced to weather in the years ahead – including around some of the most fundamental Medicaid mechanisms that hospitals rely on to provide care on a daily basis,” said MHA’s Senior Vice President of Healthcare Finance & Policy Dan McHale. “It is an especially sobering look at the peril our Health Safety Net program could face as coverage losses accelerate, with that fund already seeing record deficits that hospitals alone must absorb. That’s why this is critical time for Massachusetts to prepare and collaborate as the impacts of these federal changes draw near, and to ensure our hospitals and health systems are in a position to continue delivering high-quality, accessible care to all patients.”
The loss of premium tax credits for individuals will also harm Massachusetts as will the reduction in state-directed payments, MTF found.
“Healthcare cuts included in [OB3] will eliminate Medicaid and subsidized Connector coverage for hundreds of thousands of Massachusetts residents,” MTF concludes. “While these changes will not immediately imperil the state budget, the reduction in coverage will create a domino effect ratcheting up financial pressure on providers, increasing shortfalls within the Health Safety Net, and leading to calls for the state to stabilize healthcare finances. Given that any state approach to mitigate these financial impacts would not be eligible for federal Medicaid reimbursement, the medium-term implications of these changes are dire.”
The New Merrimack Health

One year ago, Lawrence General Hospital stepped in with the assistance of the state to rescue two Holy Family Hospitals in Haverhill and Methuen whose futures were uncertain after their parent, Steward Health Care, declared bankruptcy.
Now the three hospitals and their affiliated physician practices have rebranded under a new name – Merrimack Health.
The three hospital campuses will now be known as Merrimack Health Lawrence Hospital, Merrimack Health Haverhill Hospital, and Merrimack Health Methuen Hospital, and its community physician practices will be known as Merrimack Health Community Medical Associates. The system is led by Interim President and CEO Diana Richardson.
“One year ago, with the strong support of Governor Healey and Secretary Kate Walsh, Lawrence General and Holy Family Hospitals came together to ensure continued access to high-quality, comprehensive healthcare in the Merrimack Valley,” said Lieutenant Governor Kim Driscoll. “These hospitals and their dedicated healthcare professionals tirelessly and admirably cared for patients despite facing significant challenges. Now, we celebrate uniting these hospitals as Merrimack Health, together delivering the care that these communities deserve and that makes our state proud.”
Bipartisan Letter Seeks to Forestall DSH Cuts
Unless Congress acts, $8 billion in Medicaid funding to Disproportionate Share Hospitals (DSH) will be eliminated on October 1.
The DSH are facilities that serve a significant percentage of low-income patients, including children, the elderly, and disabled individuals. Each year, states are allotted funding that is eligible for a federal match to support care provided by DSH hospitals for low-income patients. In Massachusetts, the state’s allotment is incorporated into the MassHealth 1115 waiver and is connected to the Health Safety Net and other safety net hospital payments. The Affordable Care Act required a reduction in Medicaid DSH funding over time; however, Congress has delayed those reductions each year.
Reps. Dan Crenshaw (R-Tex.), Yvette Clarke (D-N.Y.), Gus Bilirakis (R-Fla.), and Diana DeGette (D-Colo.), in a letter to Speaker Mike Johnson (R-La.) and Democratic Leader Hakeem Jeffries (D-N.Y.), note that Medicaid DSH payments are used to help offset underpayments and uncompensated care to those facilities that qualify for the program.
“Under current statute, the Medicaid DSH program will be reduced by $8 billion in FY 2026,” reads the letter, which is currently circulating through Congress in an effort to gather more signatures. “Cuts of this magnitude would decimate the program, reducing the size of the annual allocation by more than half. Our hospitals are already under increasing financial strain, and reductions of this size would push vulnerable rural and other safety net hospitals—and the patients they serve—into peril.”
According to the non-partisan Medicaid and CHIP Payment and Access Commission, the Massachusetts DSH allotment would be reduced by $786 million, or 85.7% if the statutory cut is not addressed. The signatories of the letter seek a further delay during what they say is “a time of financial uncertainty for the nation’s hospitals.”
Helping the People Who Train the Healthcare Workforce
The Massachusetts healthcare system currently has thousands of unfilled positions, especially in the long-term care and behavioral health sectors. Compounding the problem is a shortage of people to provide preceptorships – or clinical training and mentoring – to people entering the health field. MHA-endorsed legislation that will receive a hearing tomorrow before the Joint Committee on Revenue aims to resolve the dual issues.
H. 3218/S.1960, An Act Establishing Tax Credits for Health Care Preceptorship, sponsored by Rep. Sean Reid (D-Lynn) and Sen. Sal DiDomenico (D-Everett), would create a state income tax credit for licensed healthcare practitioners – particularly doctors, nurses, and physician assistants – who serve as unpaid preceptors for students in clinical training programs. It incentivizes experienced clinicians to train the next generation of healthcare workers, particularly in regions where workforce shortages exist.
“There is often a shortage of preceptors as many licensed clinicians endure heavy workloads and have limited time during shifts, making it challenging for them to take on these responsibilities,” said Emily Dulong, MHA’s vice president of government advocacy & public policy, who is expected to testify tomorrow in support of the bill. “This legislation would invest directly in clinicians who want to become preceptors and encourage current preceptors to stay on. By giving preceptors an incentive, especially in areas with shortages, the bill helps develop a stronger, locally trained workforce that is more likely to stay and serve their own communities – goals that align closely with the priorities of both the legislature and the administration.”
Preserving Autonomy for Patients Making Decisions
People with intellectual and developmental disabilities certainly face challenges in life, but often, with the proper support, such individuals can have the autonomy to make important decisions for themselves.
Allowing such “shared decision-making agreements” is the focus of H.261, An Act Relative to Supported Decision-Making Agreements for Certain Adults, sponsored by Rep. Jay Livingstone (D-Boston). The bill was heard last week before the Joint Committee on Children, Families and Persons with Disabilities, of which Livingstone is the House chair.
Essentially, the legislation would set up a process and training to create agreements between certain adults (the “decision maker”) and their supporters whereby the decision-maker would be assisted in making choices about where the person wants to live; the services, supports, financial decisions, and medical care the decision-maker wants; whom they want to live with; and where the decision-maker wants to be educated and work, among other life choices.
Such supported decision-making is especially important in the healthcare sector because, currently, a person with intellectual and development disabilities must have a guardian appointed to them to make decisions when they are unable to do so. This not only robs the person of their autonomy but also causes long delays during hospital discharges since the guardian process, involving the courts, can take months. This in turn leads to delays in transferring patients from acute care settings to post-acute care, which exacerbates capacity problems in hospitals, ED boarding, and more. Support for supported decision-making agreements and this legislation were among the recommendations from the recent Transitions from Acute Care to Post-Acute Care (TACPAC) Task Force that the legislature created in 2024.
MHA’s Senior Director of Virtual Care & Clinical Affairs Adam Delmolino, the MHA representative on the TACPAC Task Force, who testified before the Joint Committee last week, said, “In any given month, there may be as many as 40 patients statewide who are awaiting the appointment of a guardian so that they may be discharged to the most appropriate level of post-acute care. The opportunity to adopt a shared decision-making agreement as an option and alternative to guardianship preserves autonomy for patients and their caregivers while supporting timely discharge decisions for adults with retained decision-making capacity.”
Mass. Legislators Concerned About 340B Rebate Program
This week, 163 bipartisan lawmakers, including Massachusetts Reps. Bill Keating, Stephen Lynch, Jim McGovern, Seth Moulton, Ayanna Pressley, and Lori Trahan sent a letter to the Department of Health and Human Services (HHS) urging it to abandon its 340B Rebate Model Pilot Program for drugs included in the Medicare Drug Price Negotiation Program (MDPNP).
The letter notes that the 340B program is essential to the financial stability of hospitals, particularly Medicare DSH hospitals, children’s hospitals, cancer hospitals, and rural hospitals. By shifting the financial burden onto hospitals, which would now pay for the drug upfront and apply to receive a rebate afterwards from the manufacturer, HHS threatens the financial wellbeing of these hospitals, the signatories write. For example, the average DSH hospital would be required to pay $72.2 million upfront. The letter also notes that the choice to include only drugs negotiated under the MDPNP may backfire, as these manufacturers may seek to recoup their losses through this rebate model.
In a related note, The 340B ACCESS Act, a bill to increase oversight and tighten restrictions on the 340B program, was reintroduced by Reps. Buddy Carter (R-Ga.) and Diana Harshbarger (R-Tenn). The bill would restrict the ability of outpatient departments to offer 340B drugs and require hospitals to regularly report on how they use the savings generated by the 340B program. The American Hospital Association and its members have strongly opposed the legislation.


 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association