The Challenge of Continuing Care Beds

INSIDE THE ISSUE
> Continuing Care Beds
> Assisting Patient Transfers
> COVID-19 PHE Continues
> FOCUS ON WORKFORCE: Holyoke
> X-Waiver Eliminated
> MLK Day
> Transition
MONDAY REPORT
Behavioral Health Bottlenecks Extend to Continuing Care Beds
Results of a recent survey from the Massachusetts Health & Hospital Association (MHA) and the Massachusetts Association of Behavioral Health Systems (MABHS) show that hundreds of patients are unable to access Department of Mental Health (DMH) services and are therefore “stuck” in hospital inpatient psychiatric units and freestanding psychiatric facilities. The situation, driven by workforce and bed shortages, represents how capacity pressures are reverberating through hospitals and every component of the healthcare system.
The MHA/MABHS report is intended to inform the ongoing collaboration between the provider community and the state to address the issue.
Some patients with severe psychiatric conditions who require DMH “continuing care” services have been waiting for more than a year for specialized care. Continuing care services are for those who “present serious psychiatric symptoms requiring extended hospital stays with levels of care beyond an acute care hospital.” Because psychiatric units are unable to transfer patients ready for discharge into DMH continuing care beds, the psychiatric units themselves are unable to accept new patients into the inpatient psychiatric beds. This, in turn, contributes to “behavioral health boarding” in hospital emergency departments and other units.
MHA and MABHS surveyed acute care hospitals with inpatient psychiatric units and freestanding psychiatric facilities twice – in December 2021 and November 2022. In November 2022, 322 patients were awaiting discharge from the psychiatric units. Of those, 266 were awaiting DMH services, and of the 266, 110 were awaiting DMH continuing care services. Of the 110 patients, 24 had been waiting for a DMH continuing care bed for more than a year.
The average length of stay while awaiting transfer to a continuing care bed is 197 days – an increase from 161 days in 2021.
Over the past 15 years, the total number of DMH continuing care beds across the state has dropped from 829 to 663, further challenging the ability to place patients. (The 663 includes 30 continuing care beds that were replaced in 2022 after needed infection control measures earlier in the pandemic took the beds offline.)
By statute, DMH must give “forensic” cases priority for its 660-plus continuing care beds. Since December 2021, when DMH was first mandated to report regularly on the availability of continuing care beds, 1,024 admissions to the beds were for forensic cases and only 43 were admissions from psychiatric units in hospitals or freestanding psychiatric facilities.
“We are seeing a ripple effect of backups throughout the entire healthcare system,” said Leigh Simons Youmans, MHA’s senior director of Healthcare Policy, who has been coordinating with MABHS, the state, the legislature, and advocates to help resolve the issue. “DMH is experiencing the same workforce and capacity problems as other providers, and we believe there are some solutions that can help alleviate these challenges.”
One of the primary solutions involves expanding the number of continuing care beds. In late December, DMH released a Request for Responses, seeking a qualified inpatient psychiatric hospital(s) to provide 65 continuing care inpatient level beds for civil admissions. The 65 continuing care beds may be all within one hospital or may be split across two hospitals, provided that the beds are on units dedicated exclusively to the state contract and that the minimum capacity for any single hospital is 30 beds.
In the longer-term, MHA and MABHS say that more community-based and “wrap-around” services will be needed so that DMH-run facilities can safely discharge patients and accept patients from inpatient units more rapidly.
“The fragility of the state’s behavioral health system means that the inability to place a few hundred patients translates into hundreds of additional behavioral patients boarding regularly in acute care hospitals as they await an inpatient bed,” Youmans said. “We are committed to being an active part of the solution and commend the Department of Mental Health and the legislature for laying the groundwork to add additional continuing care beds to the behavioral health continuum.”
State Expands List of SNFs That Will Accept All Patient Transfers
The most recent MHA Throughput Survey Report (December) shows that 1,043 patients in acute care hospitals across the state were awaiting discharge to post-acute services, which include inpatient rehabilitation facilities, long-term acute care hospitals, skilled nursing facilities, assisted living residences, and home care services. The December point-in-time survey recorded responses from just 37 of the more than 60 acute care hospitals in Massachusetts, meaning that the number of patients unable to be discharged was likely much higher than the 1,043.
The non-discharged patients are occupying beds that hospitals need to care for patients that are flooding hospitals due to an uptick in flu cases, conditions resulting from deferred care, and respiratory disorders, among a host of other ailments. More importantly, they are not getting the care they need from other specialized settings.
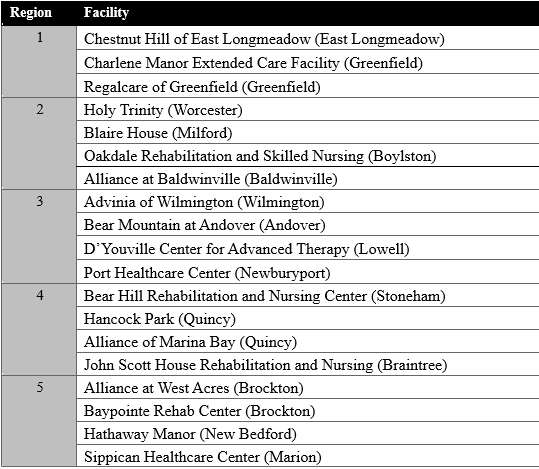
As part of the state’s continued effort to address current hospital capacity constraints and to assist with patient care transitions, the Executive Office of Health and Human Services (EOHHS), MassHealth, and Department of Public Health (DPH) last week expanded the list of nursing facilities that will accept all hospital referrals for patients that require short-term rehabilitation skilled nursing services. The state first issued a list of designated SNFs at the end of December; last week, three new facilities were added.
The above facilities must, according to the state, “be responsive to requests from any hospital for discharge planning and available to accept all new admissions, inclusive of COVID-19 positive patients, from at least 7:00 a.m. to 7:00 p.m., seven days a week.”
COVID-19 Public Health Emergency Continues
Last week, U.S. Health & Human Services Secretary Xavier Becerra once again extended the COVID-19 Public Health Emergency (PHE) declaration for another 90 days. Every 90 days since the national PHE was first declared in January 2020, the federal government has renewed the declaration. The extension was not unexpected; officials have said they will give 60-days’ notice before ending the PHE. In November 2022, when such notice was not made it became clear that the January 2023 extension would be declared. Providers say that the national healthcare workforce shortage and hospital capacity crisis, exacerbated by the winter flu season and persistent COVID-19 cases, requires that the PHE and the care flexibilities it allows be extended.
FOCUS ON WORKFORCE:
Holyoke Medical Center’s Upfront Investment in its Nursing Staff

Holyoke Medical Center has a clear-cut, attractive offer for graduate nurses: commit to work with them for four years and they’ll cut you a $50,000 check immediately upon signing if you’re coming from a baccalaureate program, or $25,000 for new nurses with an associate’s degree.
“It’s not paid incrementally, paycheck by paycheck,” says Margaret-Ann Azzaro, Holyoke’s Vice President, Patient Care Services & Chief Nursing Officer. “It’s ‘Here’s your check. We’re helping you relieve some of the stress of having to re-pay your student loans.'”
Holyoke looks for graduate nurses from inside or outside of the state who have a GPA of 3.5 or above, and who can provide their transcripts and letters of recommendation from faculty or clinical instructors. Those who are accepted into the program enroll in a six-month educational training program.
“As opposed to a new nurse coming into the hospital and just getting a 12-week orientation on one of our medical-surgical units, or a 16-week orientation on specialty units like the ED or ICU – that’s a general rule of thumb in most hospitals – in this program they also get a series of didactic classes, once a month for six months,” Azzaro says. “It’s a five-hour class that can range from developing critical thinking skills for sepsis and stroke to a range of topics such as effective communication and stress management. We have interactive skills where new nurses can practice inserting IV’s, wound care, mock code blues etc. Additionally, we incorporate journaling where we ask them, “What’s working well with the program? What kind of challenging experiences have you had? What are your thoughts about how we can make the program better?” Then we review their journaling as a group. This provides the new nurses with insight and education on new clinical issues and experiences, so that they are better equipped to deal with them in the future.
Read the rest of the story about Holyoke’s workforce strategy, as well as workplace stories from other providers throughout the state, by visiting MHA’s Workforce Toolkit.
X-Waiver Requirement Eliminated
The requirement that physicians, physician assistants, nurse practitioners, and other advanced practice registered nurses receive an X-waiver from the federal government before they are allowed to prescribe buprenorphine to treat opioid use disorder has been eliminated.
The omnibus appropriations bill that Congress passed and President Biden signed in December contained a provision to eliminate the X-waiver, so named because of the “X” that appears on the provider’s prescribing license. To get the waiver, providers had to undergo many hours of training and they were then limited to the number of patients they could treat.
Eliminating the waiver process is seen as a way to expand access to addiction treatment at a time when the opioid epidemic is not abating.
Martin Luther King Jr. Day
MHA is closed today in recognition of the federal holiday, Martin Luther King Jr. Day. The first bill proposing a federal holiday for Dr. King was introduced by Massachusetts Senator Edward Brooke (R). The holiday was signed into law in 1983 and first observed in 1986.
Last week, researchers at the Dana-Farber Cancer Institute released a study that showed once again that King’s equality efforts are yet to be fulfilled. The research showed that Black and Hispanic patients dying of cancer were less likely to receive pain-mitigating opioids than Whites near the end of life. The study of more than 300,000 patients revealed that “there are substantial and persistent racial and ethnic inequities in opioid access among older patients dying of cancer, which are not mediated by socioeconomic variables.”
But, as Rev. King said, “Change does not roll in on the wheels of inevitability, but comes through continuous struggle.” One such change that the state and MHA membership helped achieve recently was the historic revision of the Medicaid waiver that will regulate the provision of care to MassHealth recipients over the next five years. That waiver, for the first time, contains provisions that holds providers accountable for meeting targets related to health equity and clinical quality. While quality measures are a common feature of incentive-based payments, the Massachusetts waiver’s hospital health equity incentive program is unprecedented and will likely be a blueprint for other states to follow. Following MassHealth’s lead, one Massachusetts commercial insurer announced it will begin its own equity accountability effort (although it has not yet revealed details of how it will be implemented).
Transition
Al Campbell, R.N., has been named the new president of Winchester Hospital, effective March 6. He replaces interim President Matt Woods. Most recently, Campbell served as VP and COO of BJC HealthCare, which operates a 485-bed hospital in North St. Louis County, Missouri. Campbell earned his BA degree from Norfolk State University, a BS in nursing from Union College, and an MBA from the University of Phoenix.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association