BETTER CARE, LOWER COSTS: How Massachusetts Can Lead on Sensible Insurance Reform

Massachusetts Can Remove as Much as $1.75 Billion in Healthcare Spending Waste Through Sensible Insurance Reforms
Better Care, Lower Costs: How Massachusetts Can Lead on Sensible Insurance Reform highlights how unnecessary insurance practices are adding costs to the healthcare system, imposing burdens on providers, and creating obstacles for patients seeking care.
The report also offers sensible solutions for how the commonwealth can address these challenges and re-direct wasteful administrative spending to patient care.
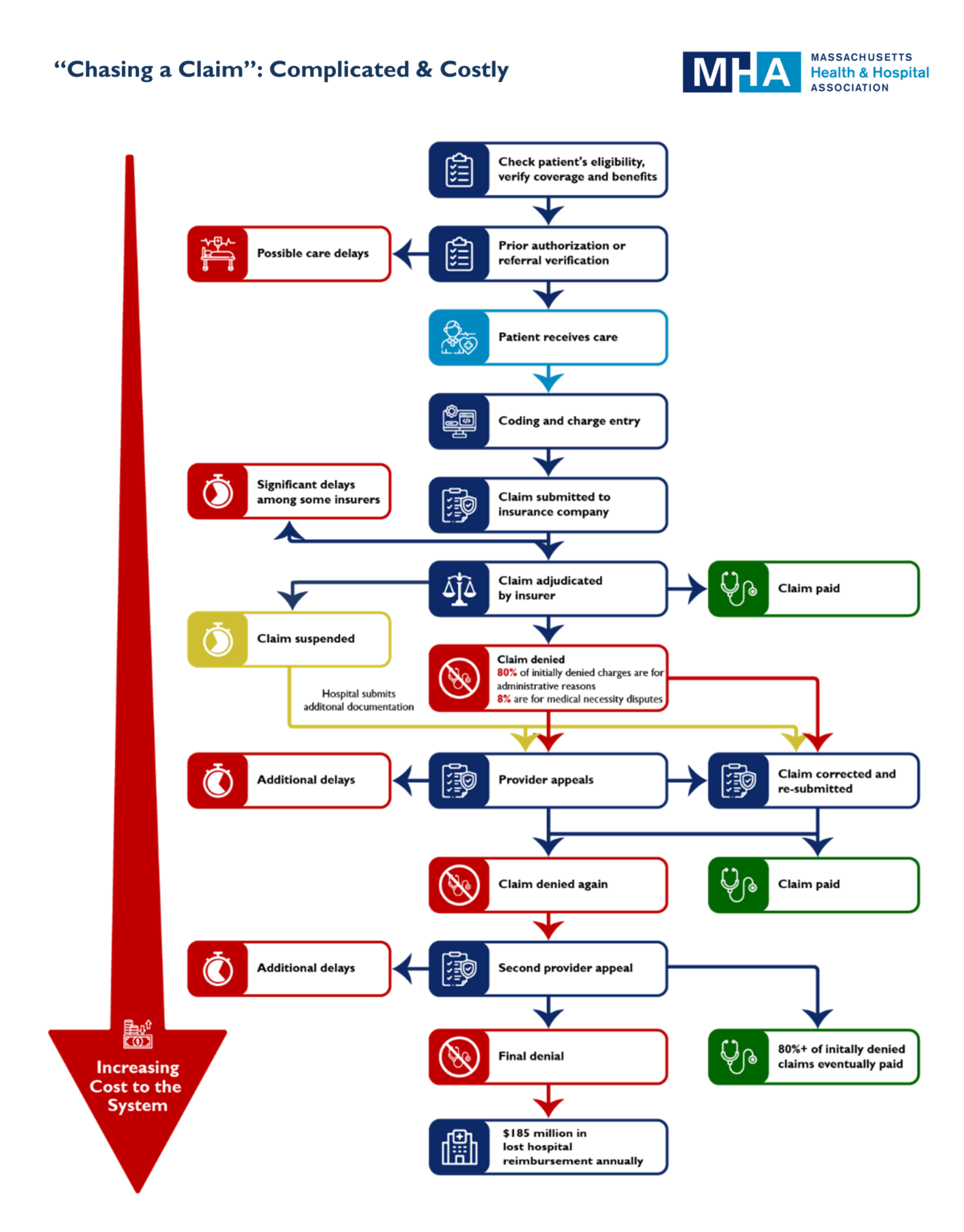
New data that MHA collected shows that each year 12% of claims that Massachusetts hospitals and health systems file with commercial insurance companies are routinely denied by the insurers – representing $1.5 billion in reimbursement for care services. More than 80% of those denied claims are eventually overturned. The process of “chasing a claim” for approval is expensive and time-consuming, using precious resources that providers could better allocate toward patient care and managing overall costs.
View the Report:
]Prior authorization disputes and excessive documentation requirements, among other insurance-related administrative burdens, are also a major cause of burnout in the healthcare profession.
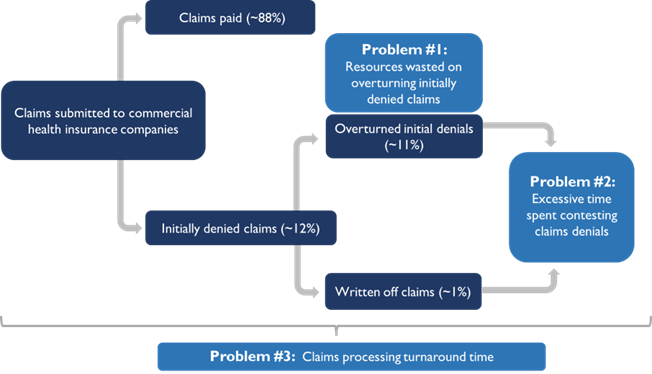
Through a series of recommended actions outlined in the report, as much as $1.75 billion could potentially be saved in the state’s healthcare system, while in turn improving affordability and access to care. The report focuses on three key problem areas and their drivers: wasted resources expended while attempting to reconcile denied claims; excessive time spent contesting claims denials; and claims processing delays.
To address these immediate concerns, MHA highlights a set of policy and legislative recommendations that would increase efficiency and reduce costs for patients and providers.
The costs and stresses brought about by certain insurance practices – particularly prior authorizations – have been the subject of increased attention both locally and nationally. In Massachusetts, the Health Policy Commission, state legislators, and a coalition of healthcare providers and advocates are leading the charge to reduce administrative burdens.
MHA members continue to report that unnecessary “red tape” insurance processes only worsen the pressures brought on by the COVID-19 crisis, including staff burnout and capacity constraints. As a result of delays and denials, 42% of claims in hospital “accounts receivable” on average remain unpaid for 90 days or longer. These delays – and the resulting costs that healthcare organizations must absorb – drain providers’ resources and are an impediment for affordable care.
“Massachusetts is a leader in innovative cost reform, and we know that every part of the system has a role to play – providers included,” said Michael Sroczynski, MHA’s senior vice president and general counsel. “As our healthcare community grapples with the long-term challenges borne out of the pandemic, reforming insurance practices is an immediate and highly effective way to ease the burden on caregivers and make care more affordable for patients. This is yet another area in which our commonwealth can lead. And we can do it in the here-and-now. We look forward to our continued work with policymakers and partners across the healthcare system in our shared mission to control costs and strengthen our world-class healthcare system for all patients.”
Key Graphic:

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association