Long-Term Care Report; New Safety Net Numbers

INSIDE THE ISSUE
> Safety Net Shortfall Spikes
> Long-Term Care Recommendations
> ED Boarding
> Surgical Mortality Rates Fall
> Steward: One Year Later
> 340B Rebates
MONDAY REPORT
Health Safety Net Shortfall’s Record Deficiency
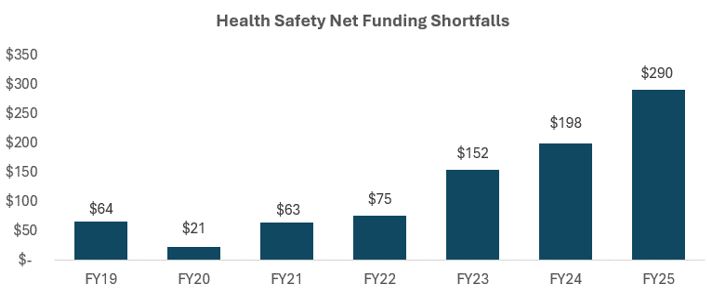
The Health Safety Net program, which funds the care that low-income, uninsured, and underinsured patients receive at hospitals and community health centers, is on track for a record-breaking funding shortfall in fiscal year 2025, which ends on September 30.
Earlier this year, MHA projected a $230 million funding shortfall in the program. The latest spending through July shows the program’s deficiency already has surpassed this mark. With two months remaining in the program’s fiscal year, the funding shortfall is anticipated to be approximately $290 million. These deficits are shouldered solely by hospitals, which already are struggling to operate on negative or razor-thin margins.
While the final FY2026 state budget did not include additional funding for the safety net, the legislature has indicated its strong commitment to hospital financial relief. Over the past few months, both the Massachusetts House and Senate have put forward safety net relief proposals for hospitals in different versions of the state budget process. House and Senate leadership, in partnership with the hospital community and Healey-Driscoll administration, continue to discuss potential relief options for the immediate FY2025 funding problem. The administration also has worked collaboratively with hospitals to identify potential solutions to mitigate the shortfalls in future years.
MHA Senior Vice President, Healthcare Finance & Policy Dan McHale said, “Addressing this immediate problem that affects every single Massachusetts hospital – as well as the patients they serve – is of the highest priority. Without relief, hospitals will be forced to absorb these untenable losses on top of the extreme cost pressures they already are experiencing. While Medicaid financing will become more challenging in future years due to the recent activity in Washington, D.C., we still have the opportunity now to maximize financial support for this critical component of our healthcare system. MHA and our member hospitals are grateful to the House, Senate, and Healey-Driscoll administration’s commitment to supporting our healthcare safety net programs and the viability of patient care services.”
Task Force Underscores Urgency to Address Capacity Constraints
A task force created under the 2024 Act to Improve Quality and Oversight of Long-Term Care has released its legislatively mandated report and recommendations on how to create a more cohesive continuum of care and resolve the issue of patients being stuck in hospitals to ensure they get to the next level of care in a timely and safe manner.
The 17-member Massachusetts Transitions from Acute Care to Post-Acute Care (TACPAC) Task Force was chaired by Executive Office of Health and Human Services Assistant Secretary Joanne Marqusee and was made up of representatives from across the hospital and healthcare field.
The law, task force, and report came about as Massachusetts confronts head-on the fact that its healthcare system regularly has approximately 2,000 patients who remain hospitalized each day despite being medically ready for discharge. (MHA’s monthly hospital throughput survey was cited in the report.) Those backups reverberate through the system, resulting in patients boarding in emergency departments (see story below) or foregoing care rather than waiting, and more than $400 million in annual losses for hospitals.
“The problem is multi-faceted and often driven by one or more of the following: legal and decision-making challenges, post-acute care capacity constraints, payer-related complexities, fragmented care coordination, complex needs, and non-emergency transportation challenges,” the task force wrote.
Specifically, the report notes:
- Patients often lack a legally authorized decision-maker—such as a guardian or Health Care Proxy—which can delay care planning and discharge;
- Post-acute capacity is affected by workforce shortages, limited availability for patients with complex needs, “and the need for more flexible service models such as hospital-at-home, mobile integrated health, remote patient monitoring, telehealth, or co-located care options;”
- “Insurance related challenges” such as prior authorizations and out-of-network placements inhibit care transfers (see surgical mortality story below);
- Patients experiencing behavioral health needs, homelessness, dementia, or interactions with the criminal justice system are especially affected, as are those who need specialized programs such as psychiatric care in a skilled nursing facility, group living environments, bariatric equipment and care, and long-term care in a nursing home; and
- Reliable transportation from one care site to another is often lacking and delayed.
The law that created the task force also took steps to resolve the issue, by mandating timely prior authorization replies and by requiring the Division of Insurance to develop a standard prior auth form, among other steps. The state also has a discharge support team to assist insurers and providers with the toughest cases.
The core of the report focuses on the next steps the state and healthcare system can take to further advance long-term care. These suggestions include many elements that MHA has proposed through legislation now pending at the State House, including bills that would expand recruitment and support of individuals to serve as guardians (H1412/S903); expanding mobile integrated healthcare programs (H1154/S726); supporting hospital-at-home care (H1141/SB806); and exploring new behavioral health transportation models that relieve the need for long-distance ambulance transport for low-risk patients (H2234/S1397).
“This report recognizes that hospitals across Massachusetts are continuing to face challenges discharging patients who are medically ready to transition to post-acute care settings,” said MHA’s Senior Director of Virtual Care & Clinical Affairs Adam Delmolino, a member of the task force. “These delays contribute to hospital crowding and suboptimal care transitions, underscoring the need for better coordination, infrastructure, and system accountability – especially as the population continues to age. The recommendations reflect the necessity to work in partnership across the care continuum and with the state to explore and implement solutions that can allow our patients to move safely, seamlessly, and efficiently through the healthcare system.” Delmolino praised the actions to date by the Healey-Driscoll administration and the legislature and urged passage this session of the provisions recommended in the report that can help resolve the patient transfer and capacity crises.
Other TACPAC members from the hospital community included Shauna Dube, senior project manager, post-acute care strategy & flow initiatives, UMass Memorial Medical Center; Tracy Lee, associate chief nurse, ambulatory & emergency services, Beth Israel Deaconess Medical Center; and Mary McClintock, associate chief nursing officer for care progression, South Shore Health.
ED Boarding is an Issue; New Report Shows When and Why
A new study that analyzed 42.6 million patient medical records in 1,700 hospitals across the U.S. has revealed some new facts about the persistent problem of patient boarding in emergency departments.
“Hospital ‘Boarding’ Of Patients In The Emergency Department Increasingly Common, 2017–24,” in the June issue of Health Affairs (subscription required), found that such boarding beyond the Joint Commission-recommended four hours has become increasingly widespread.
The study was co-authored by researchers from Veterans Affairs Ann Arbor Healthcare System and University of Michigan, as well as Beth Israel Deaconess Medical Center in Boston.
“Boarding is a key indicator of hospital capacity strain; its sustained increase portends dangerous clinical conditions during future pandemics or other disasters,” the researchers wrote. While they found that ED boarding is greatest in the winter, they add that the sustained yearly increase “suggests that factors beyond winter waves of respiratory illness are at play.”
“At a recent summit on boarding and crowding in emergency care, convened by the Agency for Healthcare Research and Quality, participants emphasized the need for real-time bed tracking systems, coordinated and regional management of limited hospital-based resources, and payment and regulatory reform,” the paper notes. “Voluntary hospital quality measure reporting and proposed hospital-based surveys for boarding are not sufficiently timely, comprehensive, or actionable.”
In Massachusetts, the provider community continues to advocate for reforms that can ease the boarding crunch. In addition to solutions to address the “stuck patient” crisis (see story above), health systems and patient advocates remain focused on the behavioral health boarding issue that affects more than 300 patients each month.
Surgical Mortality Dropping; Medicare Advantage Could Halt Progress
Despite some well-documented workforce, capacity, and financing challenges, United States hospitals are improving their core mission of keeping patients safe and alive, according to a new granular survey of mortality rates for surgical patients.
The study from Vizient, an independent data-driven hospital support company, found that surgical patients, whose acuity (or seriousness of their condition) has been steadily rising, nonetheless have a higher survival rate than they had before the pandemic began. Specifically, using data from the first quarter of 2024, compared to the final quarter of 2019 (just before the pandemic), shows that surgical patients had a 20% improvement in their survival rates.
The report notes: “Comparing actual mortality to expected mortality involves evaluating the actual number of deaths (observed) in hospitals against the number of deaths predicted based on models like those that the Centers for Medicare & Medicaid Services uses in its Value-based Purchasing program that account for multiple contributing factors (expected).” That observed-versus-expected mortality has been growing steadily in hospitalized patients, and now in surgical patients.
Vizient, which tracks data from hundreds of millions of inpatient and outpatient hospital visits, found that three key patient safety indicators created by the Agency for Healthcare Research and Quality improved dramatically at the same time that surgical mortality was decreasing. The three indicators are post-operative sepsis, post-operative respiratory failure, and post-operative hemorrhage. “Together, these reductions in patient safety indicators linked to mortality among surgical patients represent a key factor contributing to the overall improvement in survival rates for hospitalized surgical patients,” Vizient concluded.
But not all the news in the report was rosy. Vizient found that expected mortality for surgical patients going forward is expected to rise because patients presenting at hospitals in the future are expected to be sicker and require more complex care. Such “quaternary” and “tertiary” patient days will grow by 19% and 16%, respectively, by 2035, while lower-acuity patient days will grow modestly.
Another negative factor, Vizient found, is that the length of stay for surgical patients continues to rise – because they have no place to go post-surgery. “Surgical patients who stay in the hospital often need continued care before returning home,” the report notes. “This can include inpatient rehab or skilled nursing that help them recover. Delays in discharging patients to post-acute care are a growing problem for many patients and are a likely contributor to longer inpatient stays. These delays are often driven by prior authorization requirements or insufficient post-acute provider networks within [Medicare Advantage] plans.”
How Massachusetts Resolved Steward’s Blunder
One year ago this week, Governor Maura Healey announced that three new operators had stepped up to take control of six hospitals in Massachusetts that were at risk of closing due to the financial mismanagement and subsequent bankruptcy of their owner, Steward Health Care.
Boston Medical Center purchased Good Samaritan Medical Center in Brockton (now BMC South) and later took control of St. Elizabeth’s Medical Center in Brighton (now BMC Brighton), which Massachusetts took by eminent domain. Lawrence General Hospital purchased Holy Family Hospital in both Methuen and Haverhill, and Rhode Island-based Lifespan, now known as Brown University Health, purchased Morton Hospital in Taunton and Saint Anne’s Hospital in Fall River.
Two other Steward hospitals – Carney Hospital in Dorchester and Nashoba Valley Medical Center in Ayer – were forced to close when Steward did not receive any qualified bids for them. UMass Memorial Health has since discussed plans to open a standalone emergency facility in Nashoba Valley and nearby Emerson Health has seen an uptick in patients. Two state-commissioned working groups were formed to address the needs of the communities affected by the closed hospitals; both groups concluded that while health services in the affected areas were needed, it would not be feasible to create new hospitals where the now-closed facilities stand. Steward Norwood Hospital, which had been closed for years due to flooding, was not part of the bankruptcy proceedings. It stands uncompleted although a “Finish Norwood Hospital” campaign has been created.
The effort to get Massachusetts bidders, coordinate care until the final deals were signed, appropriate state “bridge” funding to meet payroll and keep the hospitals’ doors open, all while dealing through a Texas-based federal bankruptcy court and the intractable Steward company was a massive undertaking for both the state and the Massachusetts hospital community.
Steward possessed 31 hospitals when it went bankrupt. In addition to the two hospitals in Massachusetts, two Ohio hospitals have been closed (but may re-open) and hospitals in Arizona, Miami, and Texas have dramatically pared back services and workforce as a result of the bankruptcy.
HHS Launches 340B Rebate Model Pilot Program
At the end of July, the Health Resources and Services Administration (HRSA) announced the launch of a voluntary 340B Rebate Model Pilot Program, offering qualifying drug manufacturers a new mechanism to apply the 340B ceiling price to select drugs for all covered entities.
The initiative is designed to test the feasibility and effect of a rebate-based approach within the 340B Drug Pricing Program. The program will be limited to drugs included in the Medicare Drug Price Negotiation Selected Drug List. Participating manufacturers must commit to the program for a minimum of one year.
Applications are due by September 15, with approvals expected by October 15. The program is scheduled to take effect on January 1, 2026. The agency is also seeking public comments on the structure and application process of the pilot through September 2, 2025.
Currently, 340B entities, including eligible hospitals, purchase 340B drugs at a discounted rate from drug manufacturers. Under manufacturer-proposed “rebate models,” 340B covered entities have to buy drugs at commercial prices and then seek a rebate to meet the 340B ceiling price. HRSA claims the pilot program will give it insight into the controversial rebate issue.
Such rebates impose significant obstacles to providers in realizing the intended 340B benefit, including increased administrative burden, delayed payment, and risk of denial. The rebate model has been the subject of court cases in which hospital groups, including MHA and the American Hospital Association (AHA), have weighed in on. In its amicus brief to the Supreme Court, the hospital groups wrote, “In a world of finite resources, 340B hospitals will have no choice but to divert funds away from patient services and towards burdensome compliance. All of these consequences ‘frustrate’ the goal of the 340B statute.”


 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association